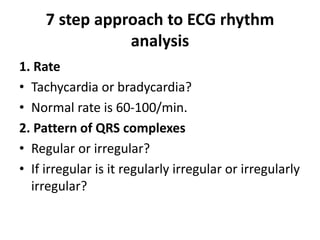
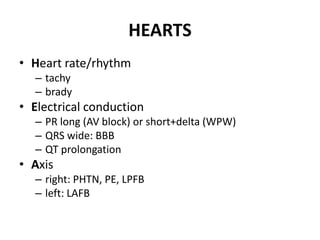
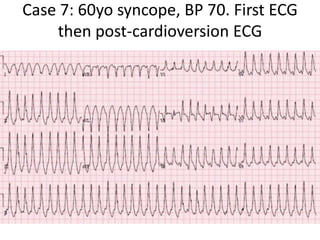
The document outlines a detailed ECG analysis methodology, which includes a 7-step approach to rhythm analysis focusing on rate, morphology, and the relationship between P waves and QRS complexes. It further categorizes various types of tachycardia and bradycardia, alongside providing case studies demonstrating ECG interpretations and potential diagnoses. Additionally, it discusses the classification of syncope and the necessary guidelines for diagnosis and management as per the 2018 ESC guidelines.