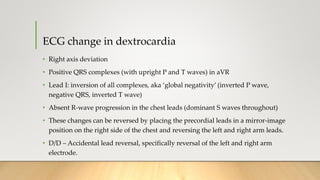
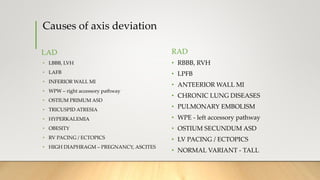
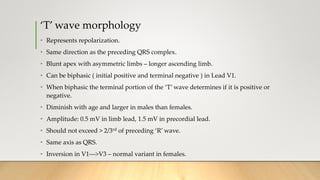
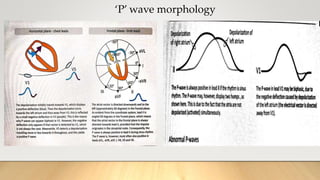
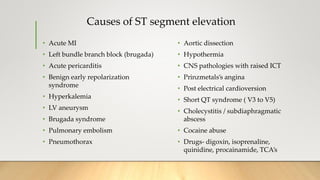
The document provides a comprehensive overview of electrocardiograms (ECGs), explaining their definition, history, types of leads, and interpretation techniques. Key topics include the sequence of electrical activation in the heart, heart rate determination methods, and various abnormalities that can be identified through ECG analysis. Additionally, it details the factors affecting ECG results, such as axis determination and common causes of changes in wave morphology.


![Contd..
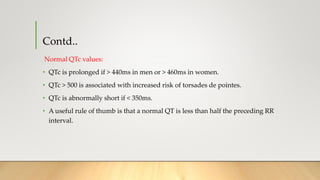
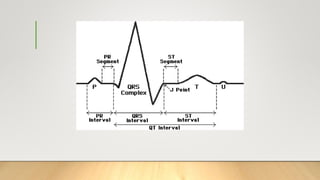
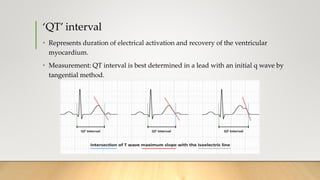
• QT interval is rate dependent. To ensure complete recovery from one cardiac
cycle before the next cardiac cycle begins, the duration of recovery must decrease
as the rate of activation increases.
• Therefore normality of QT interval can be determined only by correcting for the
heart rate ----> QTc
• Bazett: QTcB = QT/RR1/2
• Fridericia: QTcFri = QT/RR1/3
• Framingham: QTcFra = QT+0.154 (1−RR)
• Hodges: QTcH = QT+0.00175 ([60/RR]−60)
• Rautaharju: QTcR = QT−0.185 (RR−1) + k (k=+0.006 seconds for men and
+0 seconds for women)](https://image.slidesharecdn.com/ecgbasics-190206170243/85/Ecg-basics-59-320.jpg)