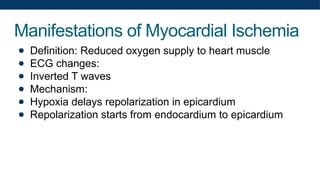
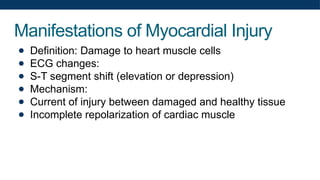
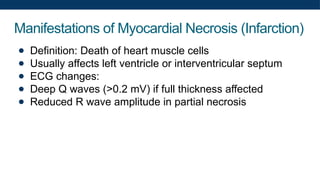
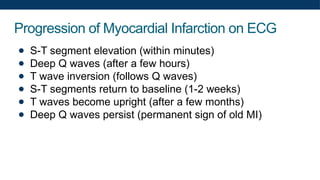
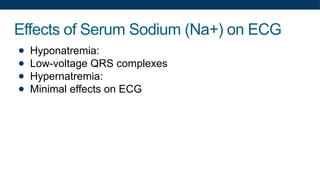
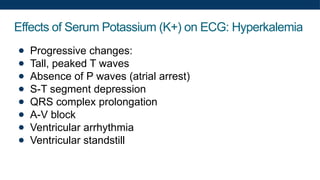
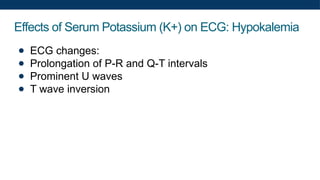
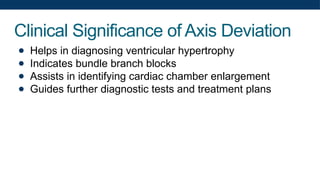
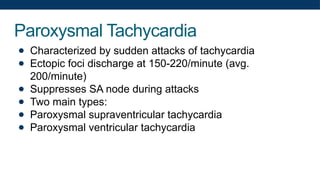
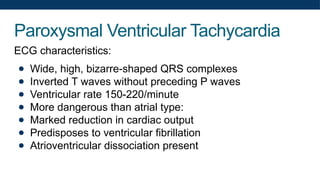
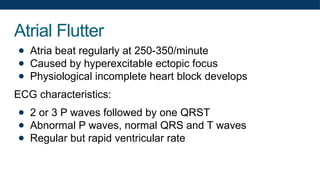
The document provides a comprehensive overview of the principles and recording of electrocardiograms (ECG), detailing the types of leads, waveforms, intervals, and their significance in diagnosing cardiac conditions. It discusses key aspects such as ECG calibration, heart rate calculation, axis deviation, ventricular hypertrophy, and the effects of electrolyte imbalances on ECG results. Additionally, it covers arrhythmias, their causes, classifications, and specific ECG patterns associated with various heart rhythm abnormalities.