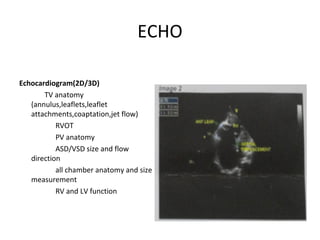
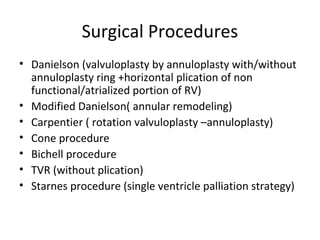
This document summarizes Ebstein's anomaly, a congenital heart defect characterized by displacement of the tricuspid valve into the right ventricle. Key features include delamination of the tricuspid leaflets, apical displacement of the tricuspid annulus, and dilation of the right atrium. Presentation varies from no symptoms to heart failure. Diagnosis involves echocardiogram and cardiac catheterization. Surgical options aim to repair or replace the tricuspid valve, with newer techniques using a cone reconstruction approach. Outcomes depend on severity, with some patients living into their 80s while others require heart transplantation.