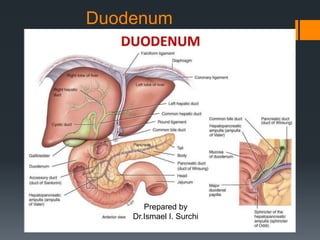
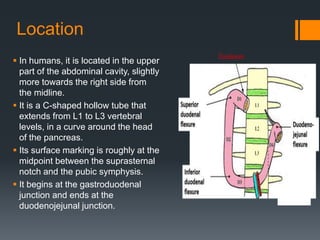
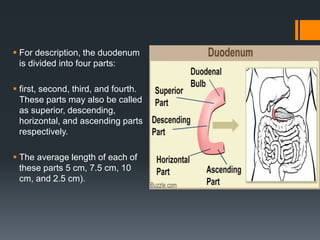
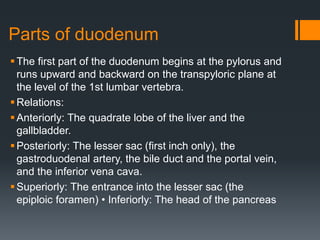
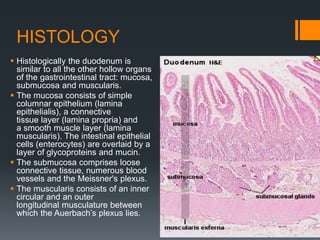
The document provides a comprehensive overview of the duodenum, covering its anatomy, histology, blood supply, innervation, physiological functions, and common conditions. It describes the duodenum's location in the abdominal cavity, its structure divided into four parts, and its role in digestion, hormone secretion, and nutrient absorption. Additionally, it addresses various conditions affecting the duodenum, such as ulcers, inflammation, and cancer.