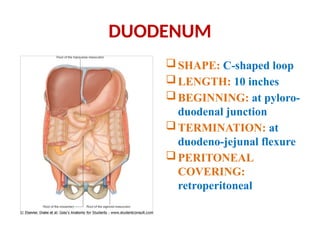
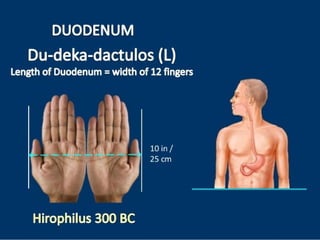
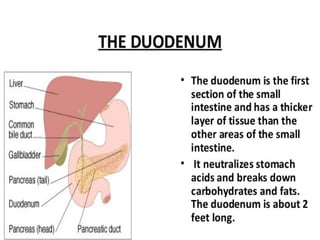
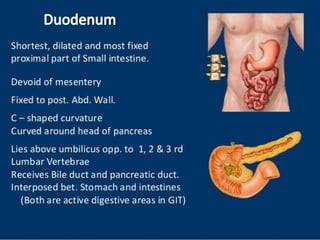
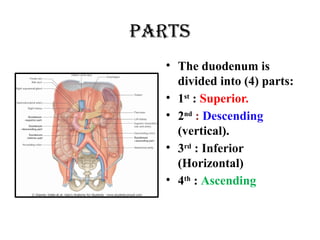
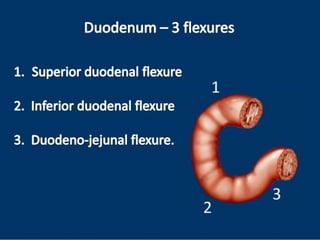
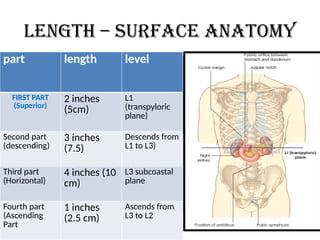
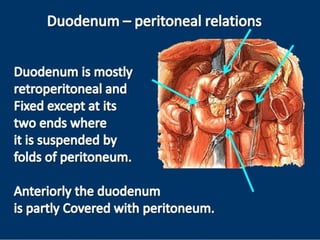
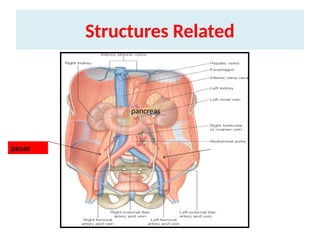
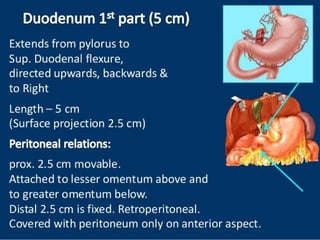
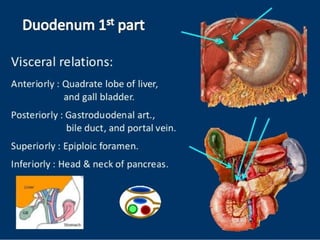
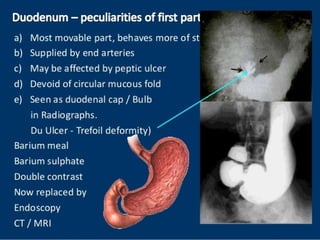
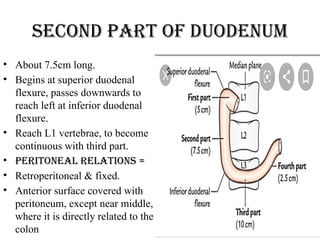
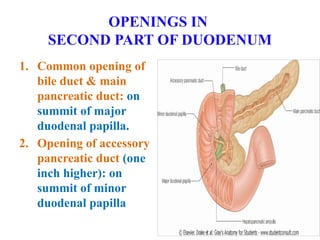
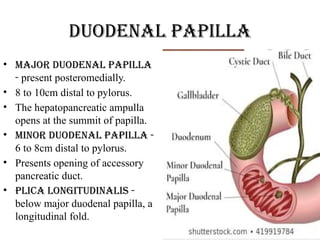
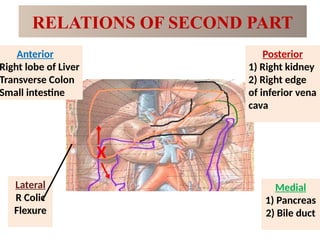
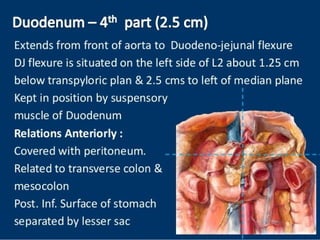
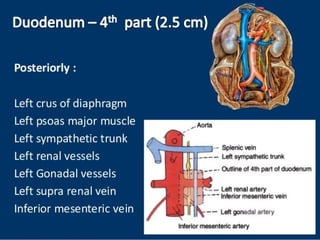
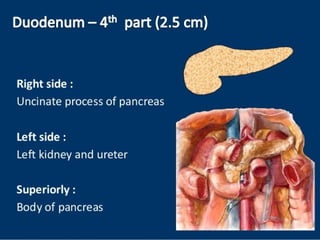
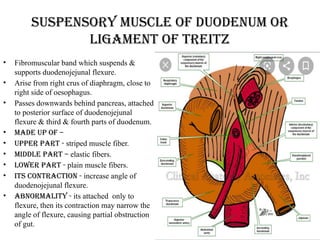
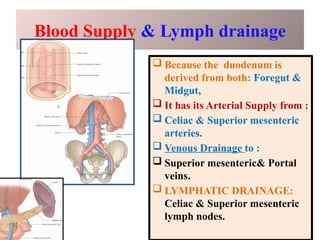
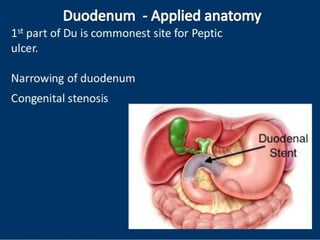
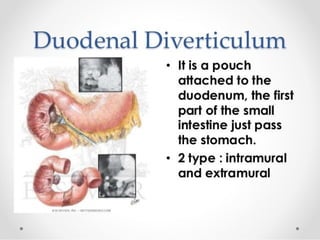
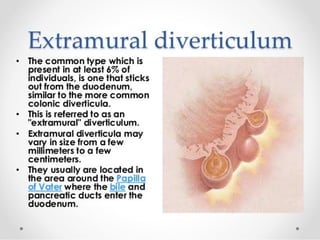
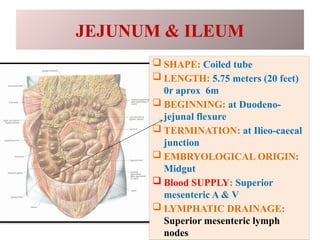
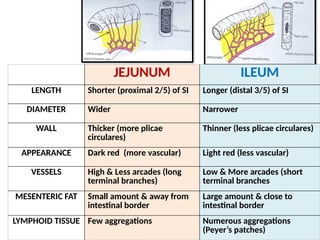
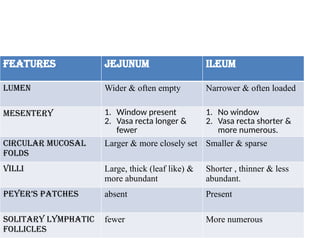
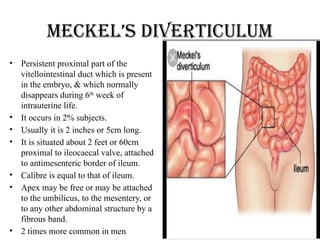
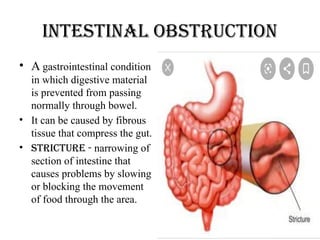
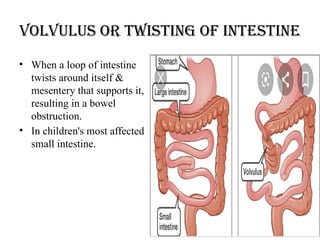
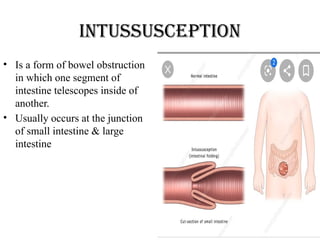
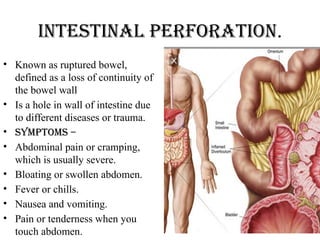
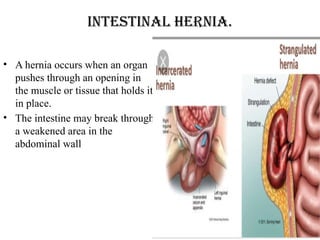
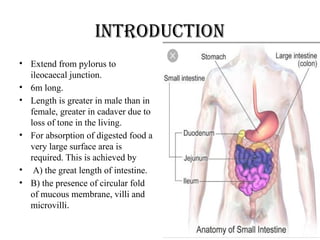
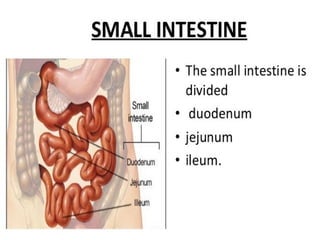
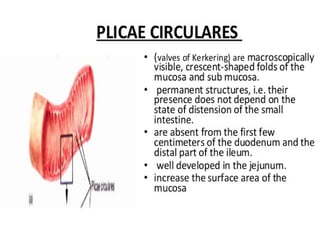
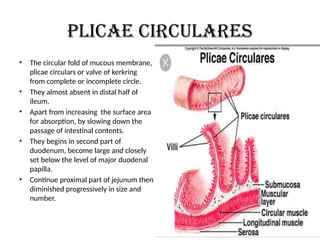
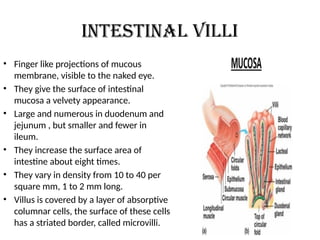
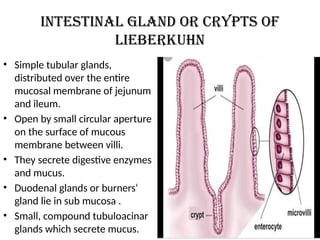
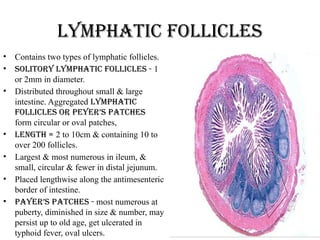
The document provides an extensive overview of the anatomy and functions of the small intestine, detailing its length, surface area adaptations for absorption, and structural components such as plicae circulares, intestinal villi, and lymphatic follicles. It also describes the duodenum's parts, their peritoneal relations, and vascular supply, as well as differences between the jejunum and ileum. Additionally, it discusses conditions affecting the intestine, such as intestinal obstruction and hernias.
![{kqnzkUr
• ^^vl`t% ‘ys”e.k’pkfi ;% izlkn% ijkser% ra iP;ekua fiRrsu
ok;q’pkI;uq /kkofrAA
rrksvL;kU=kf.k tk;Urs xqna ofLr’p nsfgu%AA** ¼lq-’kk-
4@25&26½
• vkpk;Z lqJqr ds vuqlkj jDr vkSj dQ ds lkjre Hkkx esa fiRr
ds }kjk idrs le; mlesa ok;q Hkh vk tkrh gS] rc mlls vkU= dh
yEckbZ lk<s rhu O;ke ,oa fL=;ksa esa rhu O;ke crk;h gSA
• ^^ lk/kZf=O;kekU;U=kf.k iqalk] L=h.kke/kZO;keghukfu**AA
¼lq-’kk-5@8½](https://image.slidesharecdn.com/smallintestine-250121063018-aef75ed7/85/SMALL-INTESTINE-pptx-2-320.jpg)
![xzg.kh
• ^^vXU;f/k”BkueUuL; xzg.kkn~ xzg.kh erkA
ukHks:ifj lkâfXu cyksiLrEHk c`afgrk**AA ¼p-fp-15@56½
• vkpk;Z pjd ds vuqlkj xzg.kh dks vfXu dk vkJ; gksus ,oa vUu dks xzg.k djus
ds dkj.k bls xzg.kh laKk nsrs gq, bldh fLFkfr ukfHk ds mij crk;h gSA
• ^^ iDokek’k;e/;LFkk xzg.kh lk izdhfrZrk**A ¼lq-m-40@169½
• lqJqr us Hkh vkek’k; ,oa iDok’k; ds e/; fLFkr vo;o dks xzg.kh laKk nh gSA
• ^^“k”Bh fiRr/kjk uke] ;k prqZfo/keUuikueqiHkqDrekEk’k;kr~ izP;qr
iDok’k;ksifLFkra /kkj;fr**AA ¼lq-’kk-4@17½
• vkpk;Z lqJqr us fiRr/kjk dyk dk LFkku Hkh vkek’k; ,oa iDok’k; ds e/; crk;k
gSA lsou fd;s prqfoZ/k vUuiku tks vkek’k; ls vkrk gS] mls xzg.k djus okyk
vo;o xzg.kh gSA xzg.kh esa fiRr ds }kjk vUu th.kZ gksdj iDok’k; dh vksj
ikpu ds fy, Hkst fn;k gSA](https://image.slidesharecdn.com/smallintestine-250121063018-aef75ed7/85/SMALL-INTESTINE-pptx-10-320.jpg)