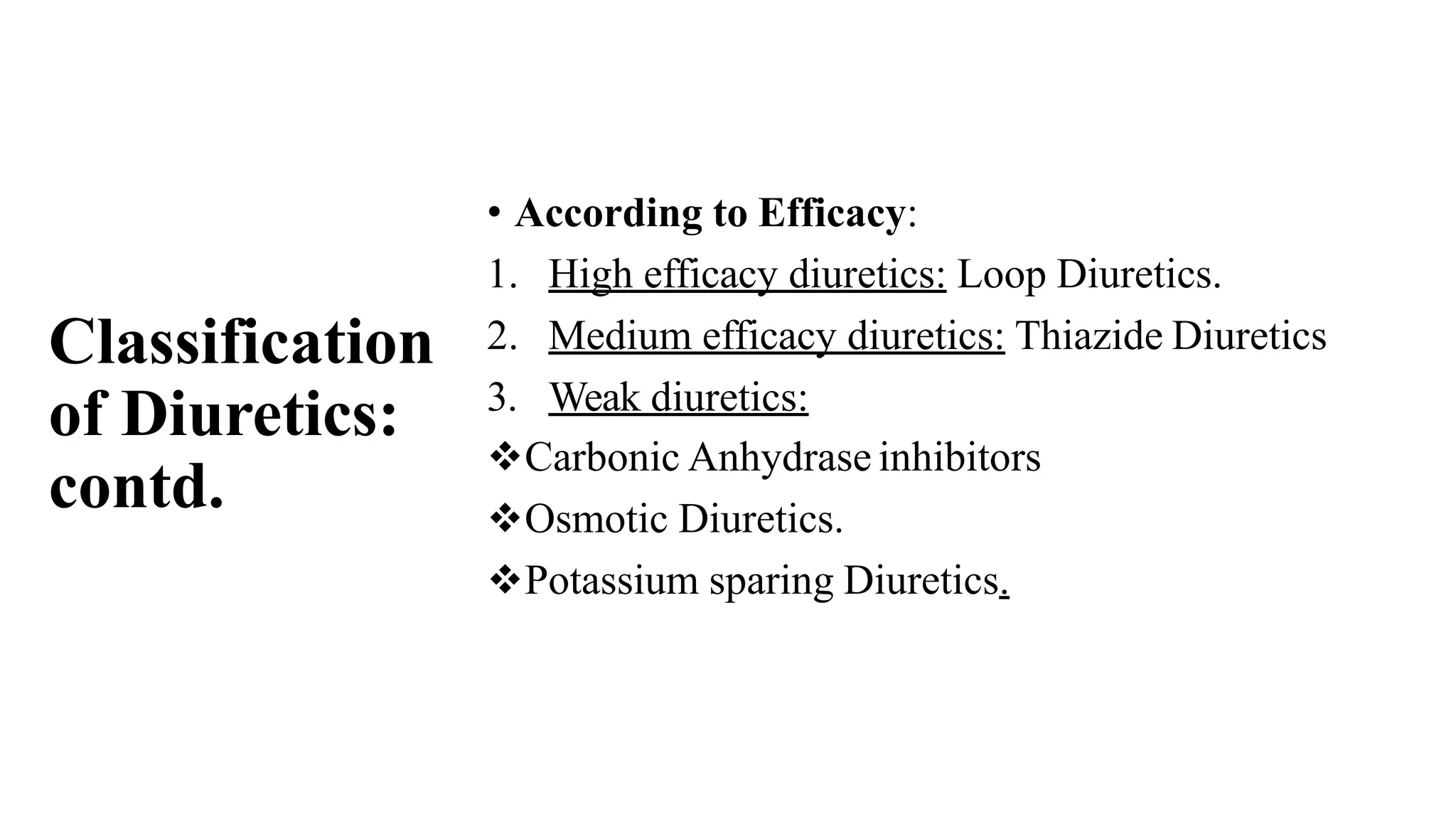
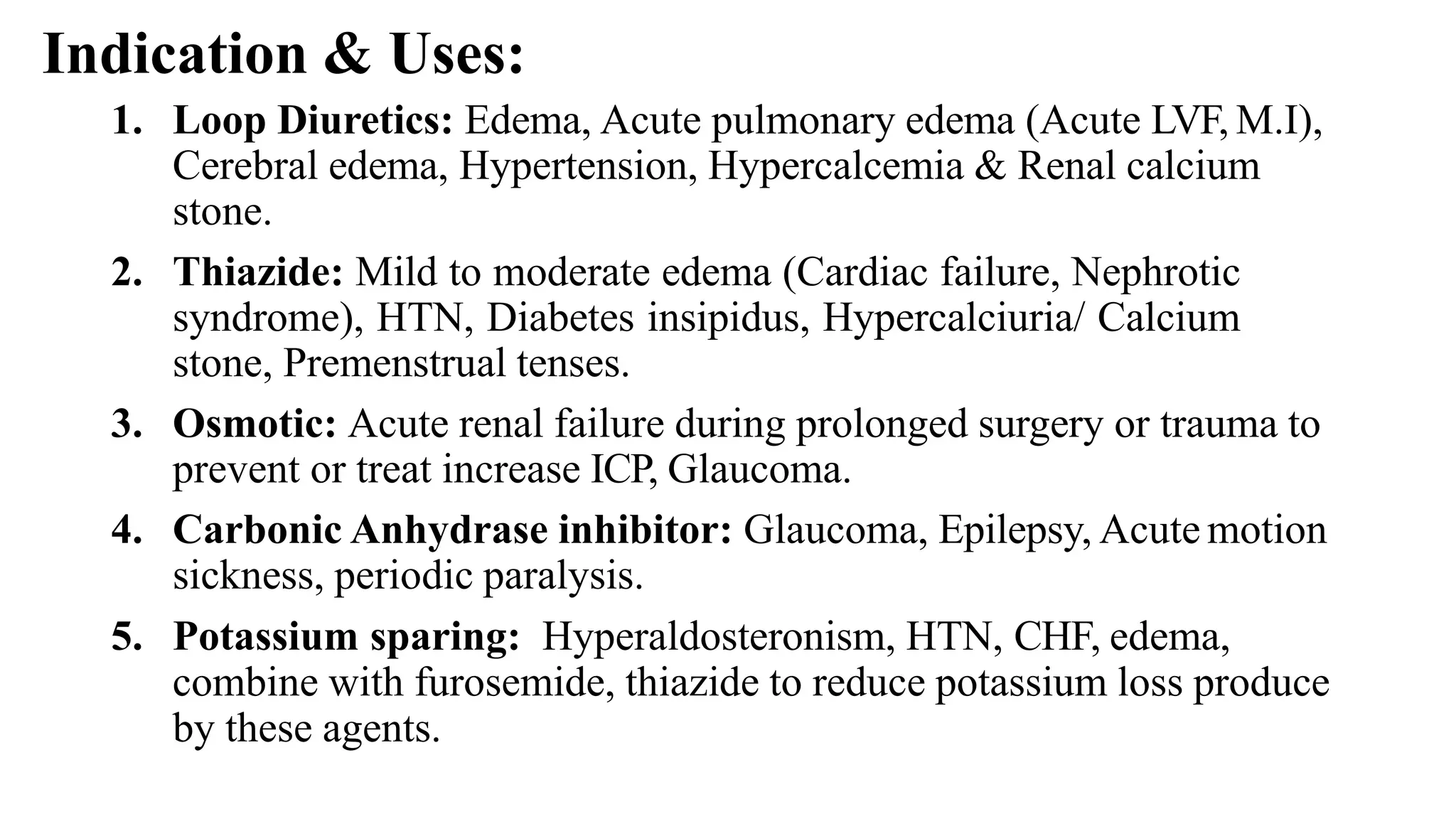
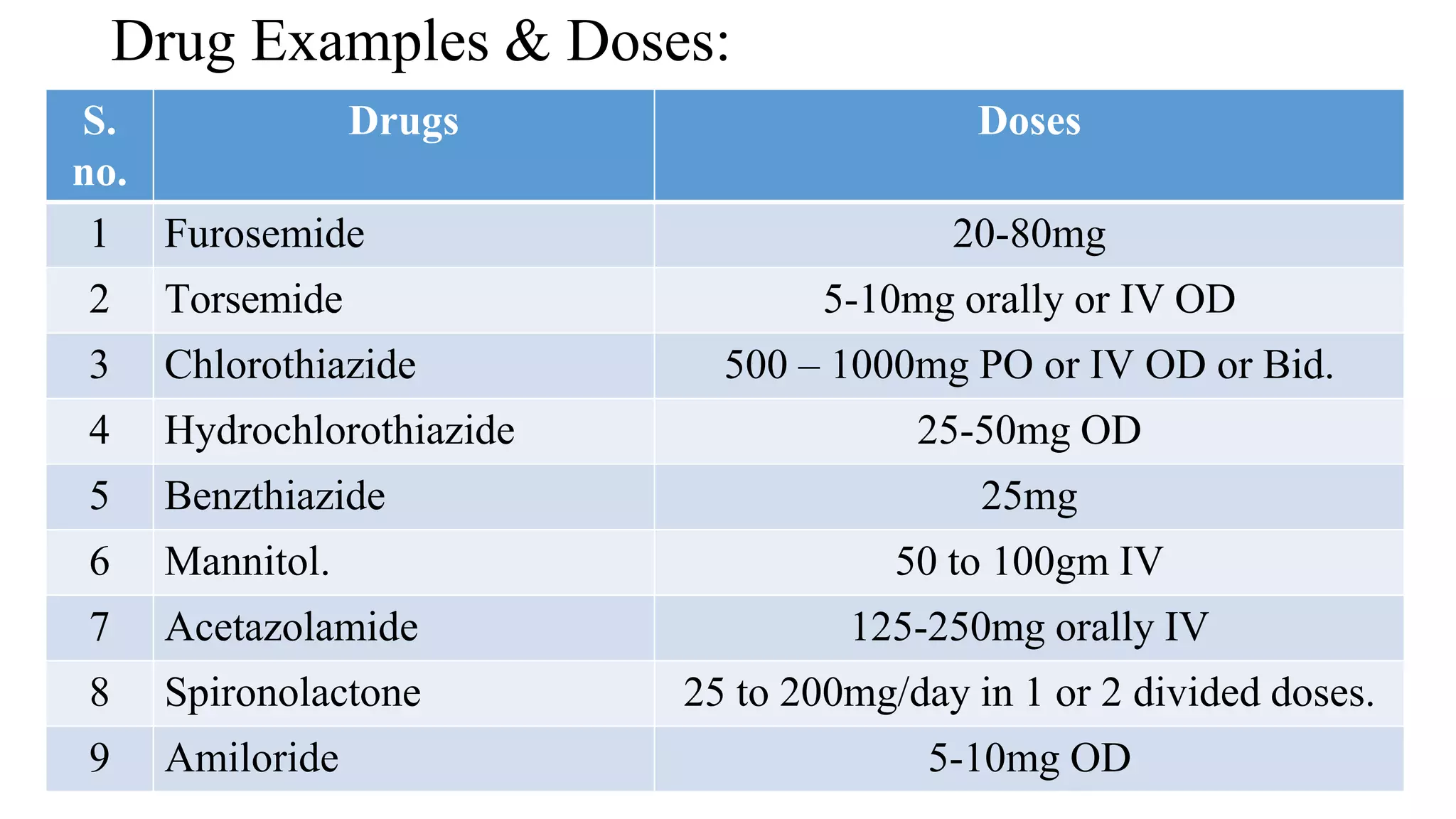
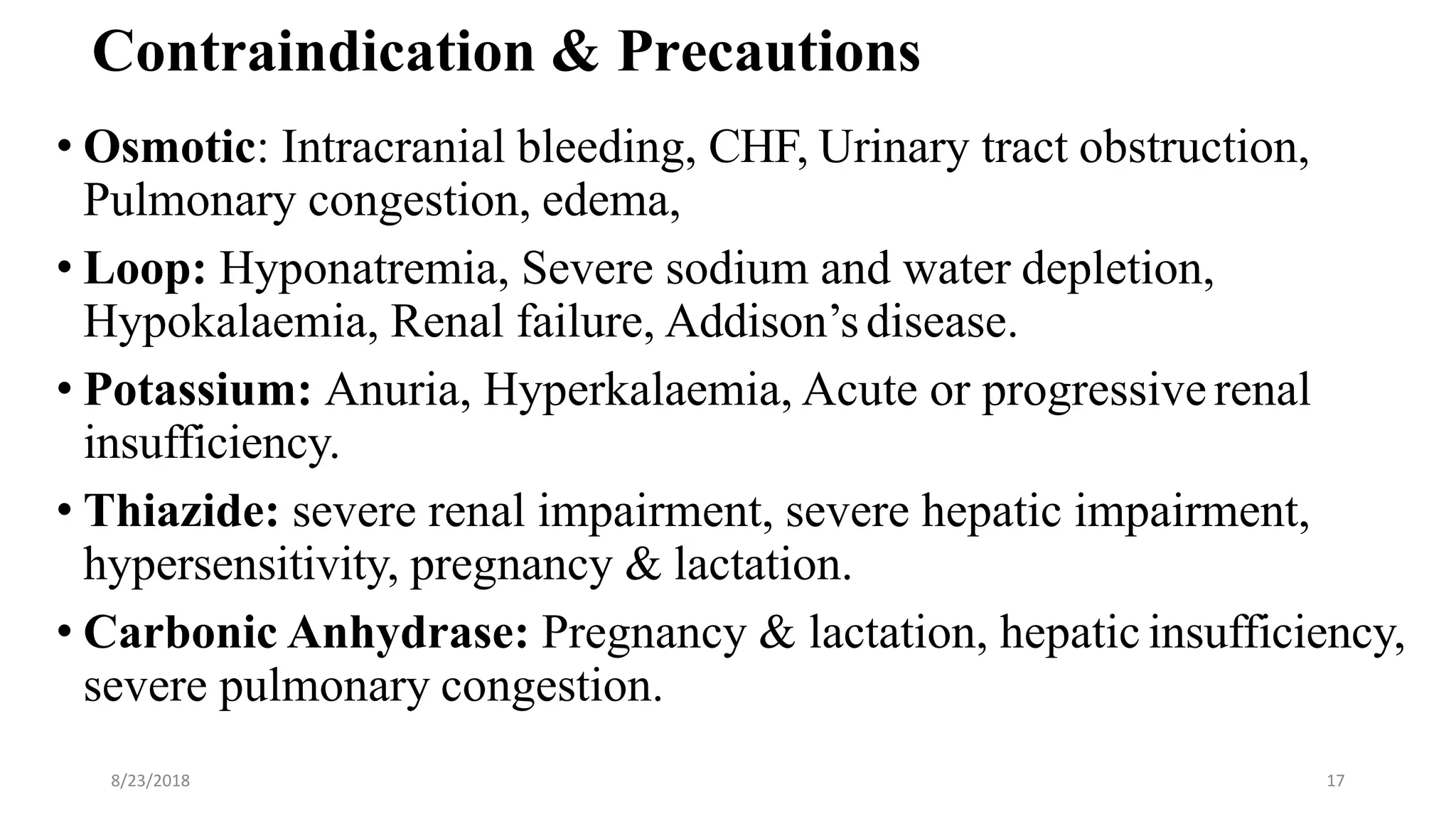
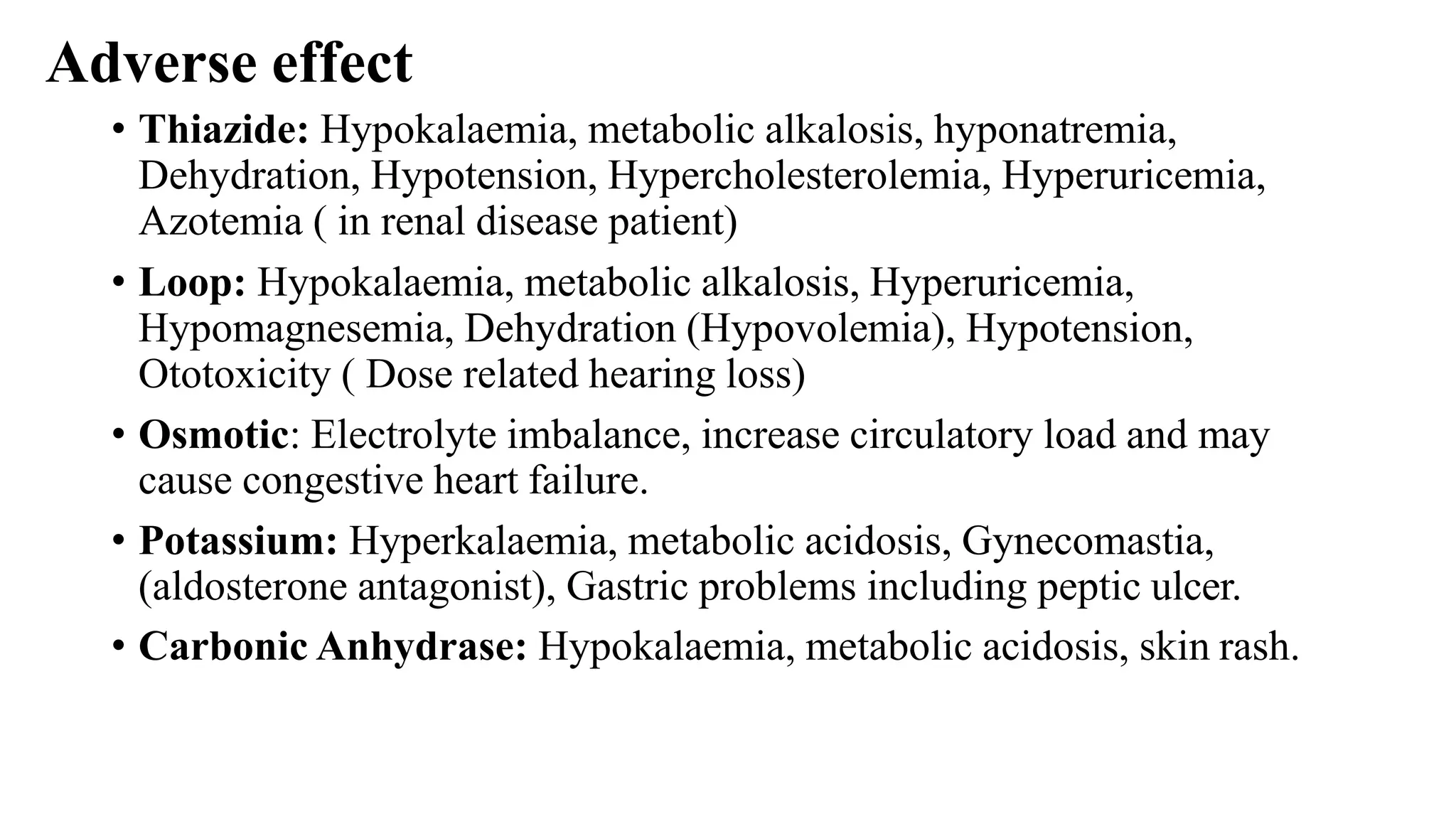
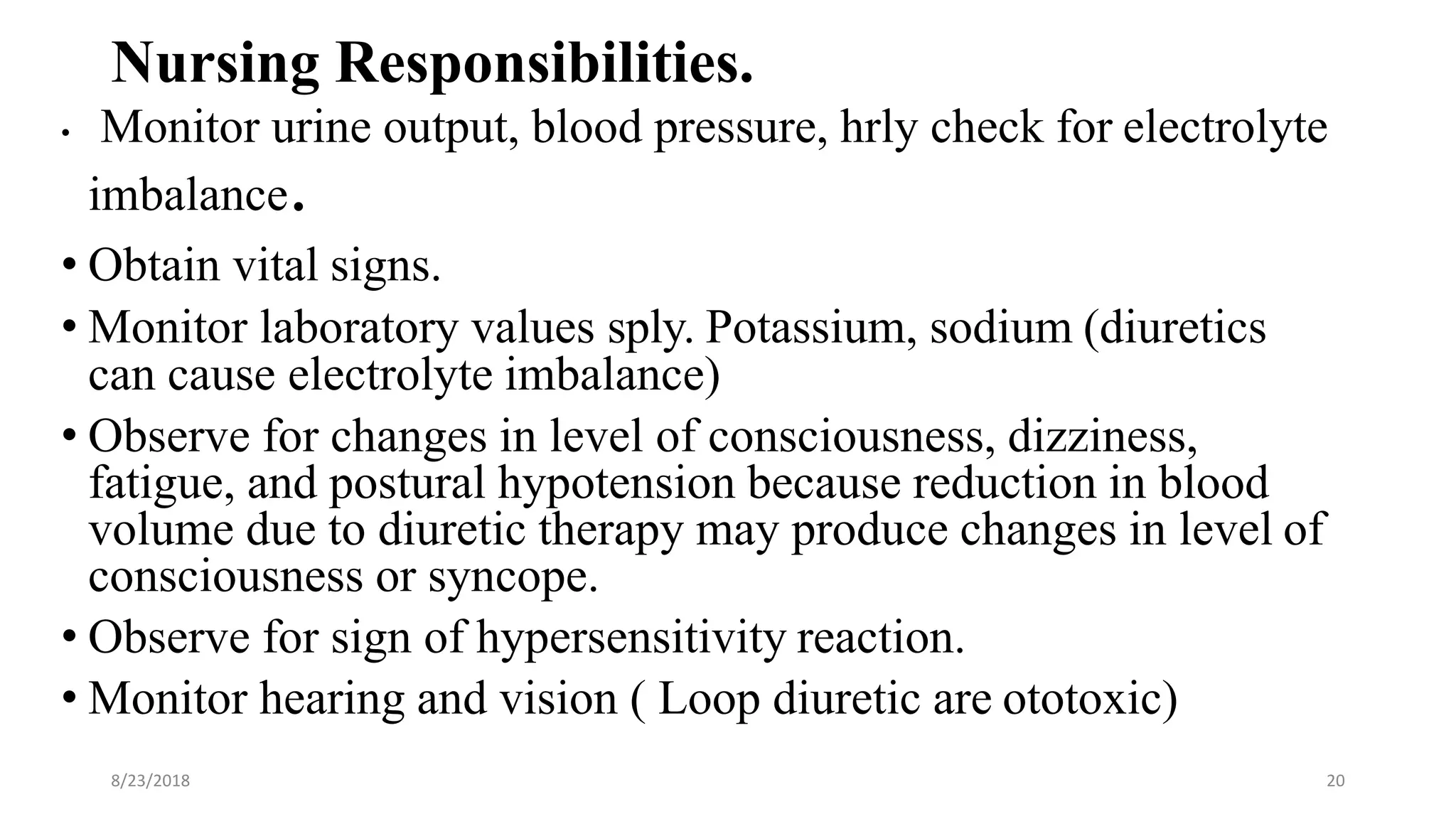
The document outlines the pharmacology of drugs used for the urinary system, focusing on diuretics, antidiuretics, and urinary antiseptics, including their classifications, mechanisms of action, indications, contraindications, and nursing responsibilities. It provides detailed information about various types of diuretics, their uses in conditions like heart failure and hypertension, as well as adverse effects and potential drug interactions. Additionally, it covers the role of urinary antiseptics in treating infections and highlights critical nursing practices for monitoring and patient education.