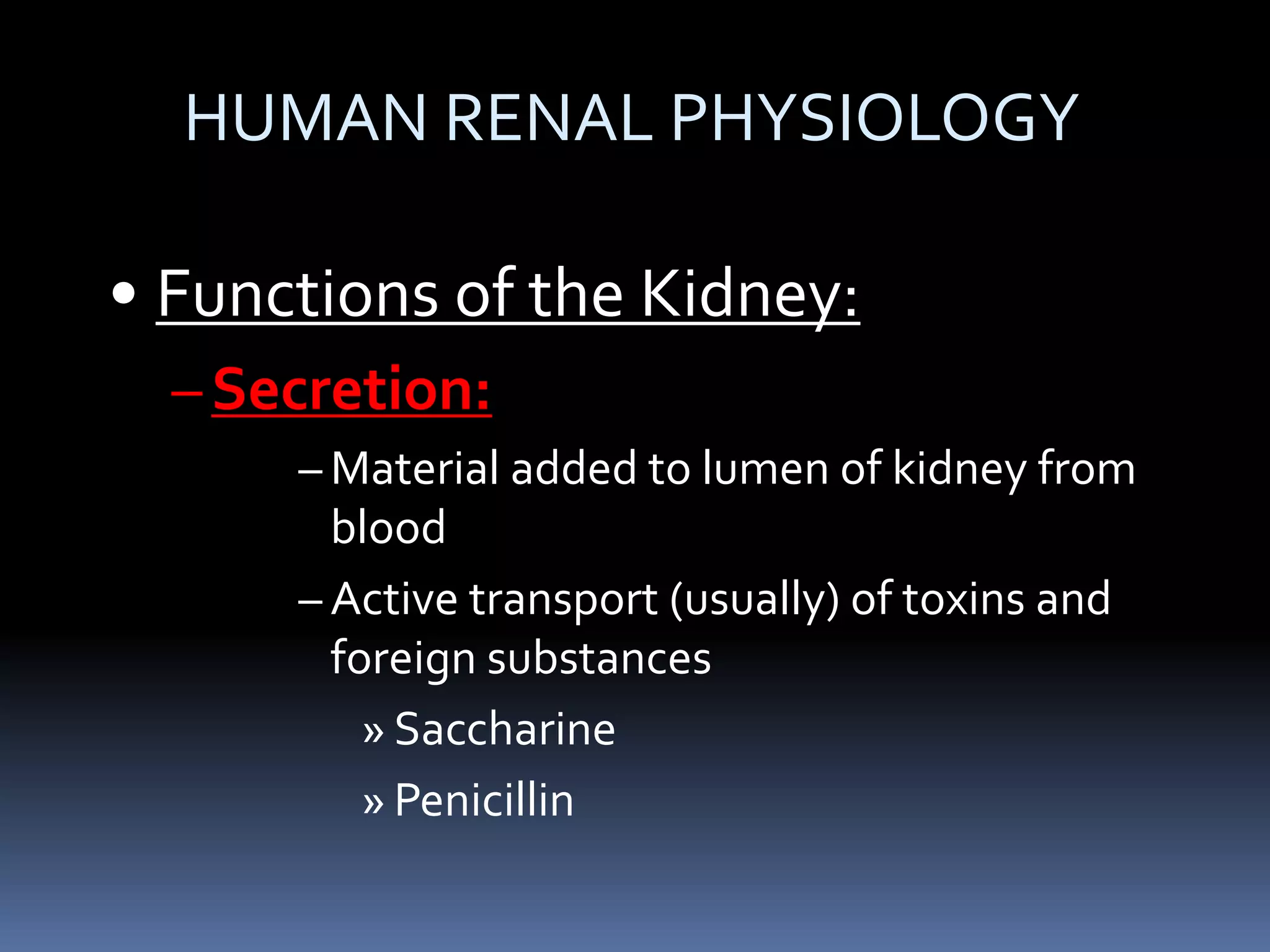
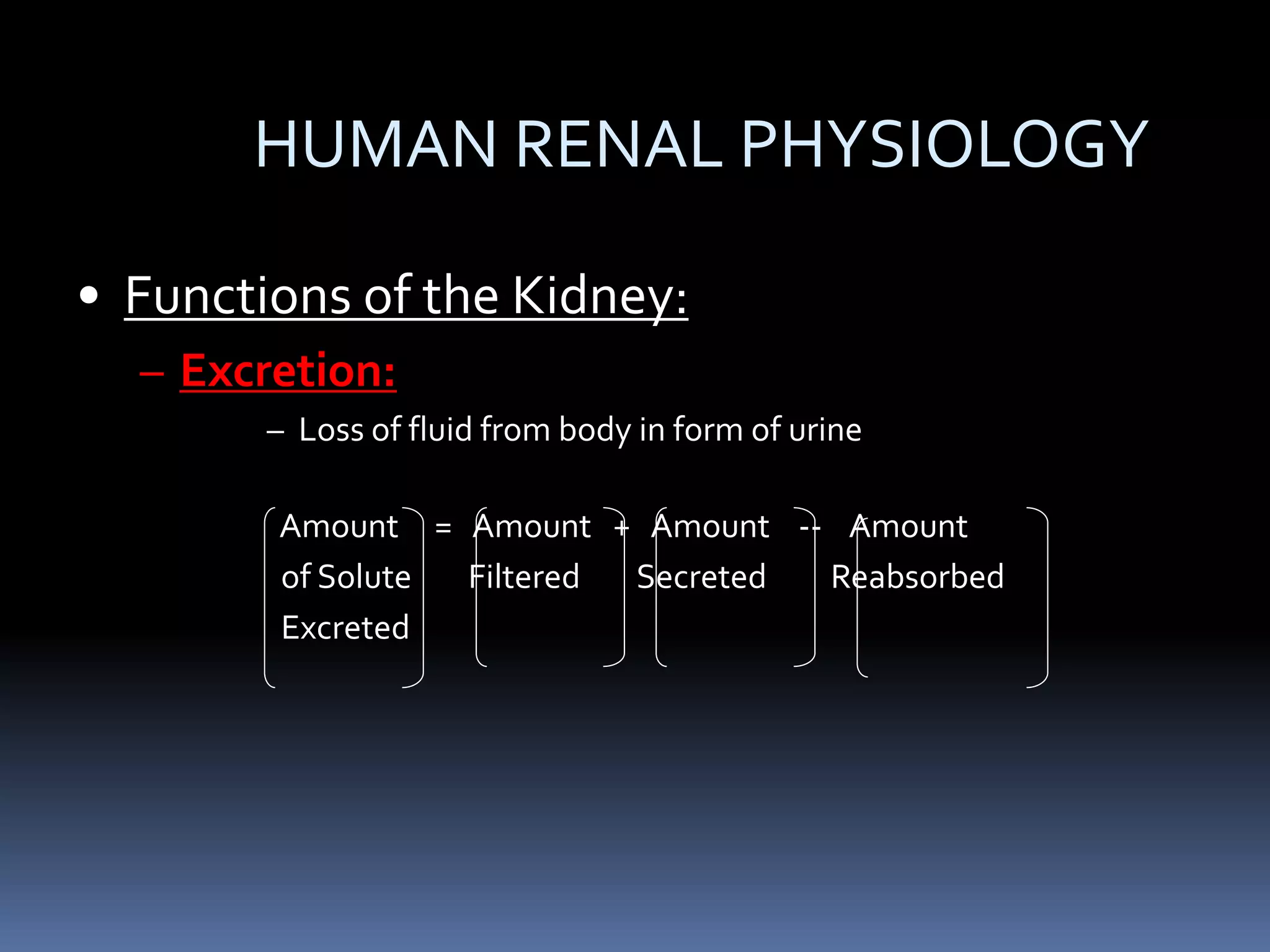
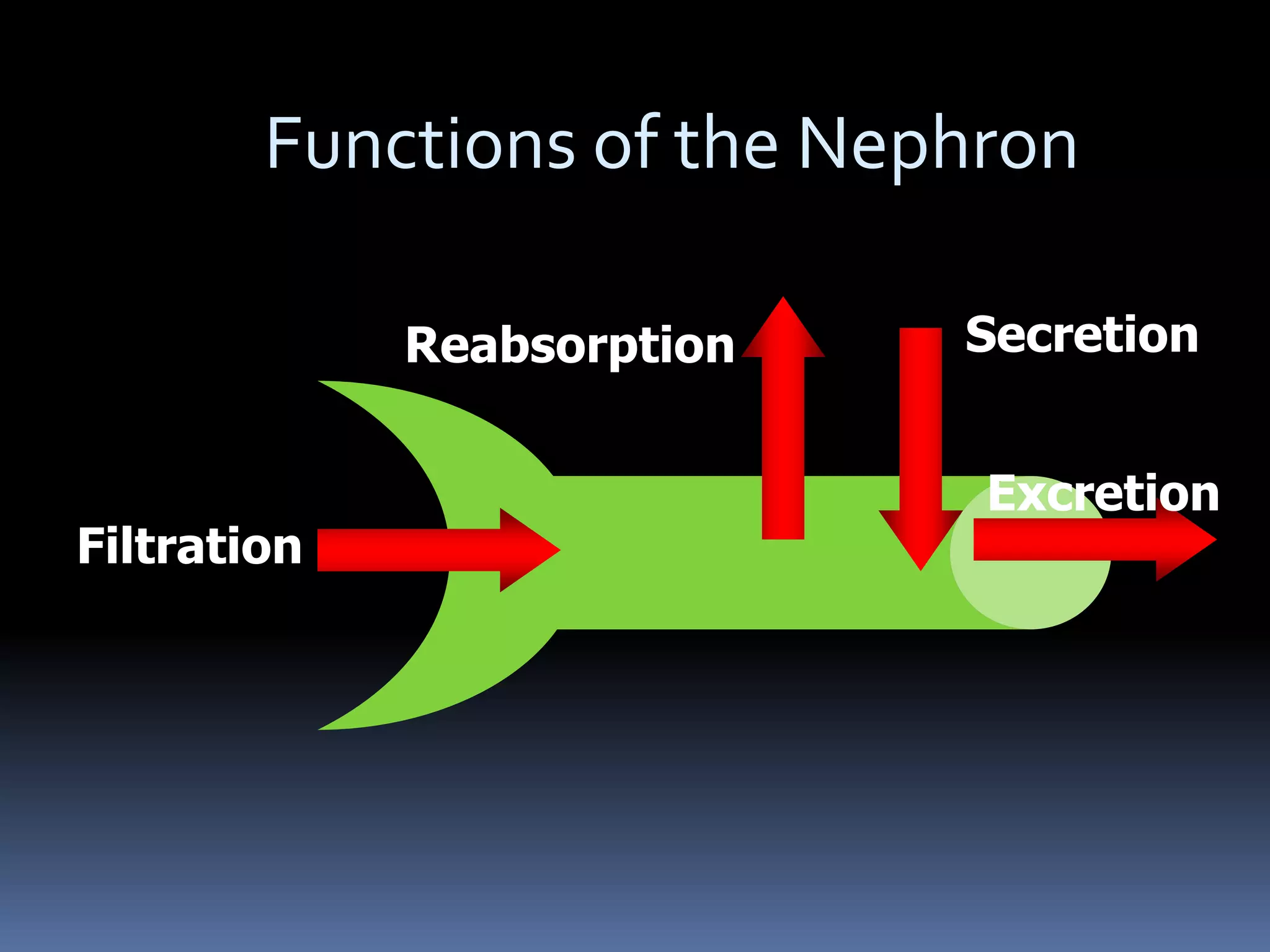
The document discusses human renal physiology and diuretics. It covers the key functions of the kidney - filtration, reabsorption, secretion and excretion. It then describes different types of diuretics and how they work, including loop diuretics, potassium sparing diuretics, high ceiling diuretics, osmotic diuretics, thiazide diuretics and carbonic anhydrase inhibitors. Potential side effects of diuretic use are also outlined. The document concludes by discussing antidiuretics like ADH/vasopressin and synthetic forms like desmopressin, as well as lythotriptics and hepatoprotection.
![Hepatoprotection
Hepatoprotection or antihepatotoxicity is the
ability to prevent damage to the liver.
The liver plays a central role in transforming and
clearing chemicals and is susceptible to the
toxicity from these agents. Certain medicinal
agents, when taken in overdoses and sometimes
even when introduced within therapeutic ranges,
may injure the organ.
More than 900 drugs have been implicated in
causing liver injury[1] and it is the most common
reason for a drug to be withdrawn from the
market.](https://image.slidesharecdn.com/diuretics-ppt-200610015617/75/Diuretics-ppt-for-BAMS-students-22-2048.jpg)
![HEPATOTOXICITY
. Several mechanisms are responsible for either
inducing hepatic injury or worsening the damage
process. Many chemicals damage mitochondria, an
intracellular organelle that produce energy. Its
dysfunction releases excessive amount of oxidants
that, in turn, injure hepatic cells.Activation of some
enzymes in the cytochrome P-450 system such as
CYP2E1 also lead to oxidative stress.[12] Injury to
hepatocyte and bile duct cells lead to accumulation of
bile acid inside the liver.This promotes further liver
damage.[13] Non-parenchymal cells such as Kupffer
cells, fat storing stellate cells, and leukocytes (i.e.
neutrophil and monocyte) also have a role in the
mechanism.](https://image.slidesharecdn.com/diuretics-ppt-200610015617/75/Diuretics-ppt-for-BAMS-students-23-2048.jpg)