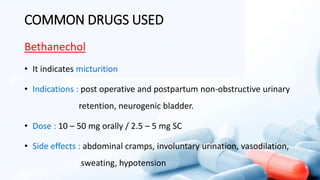
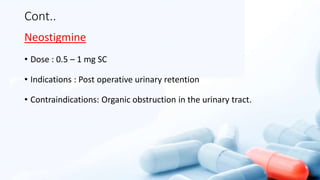
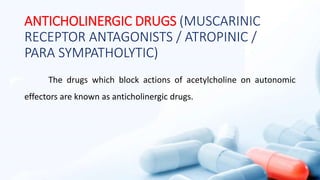
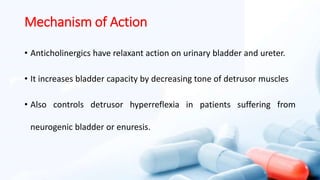
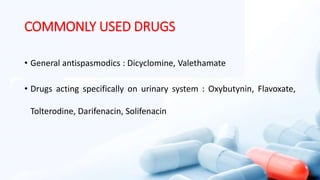
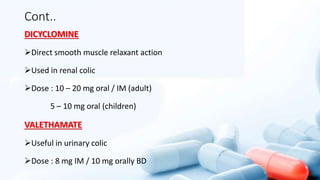
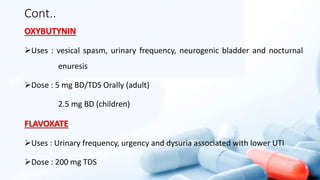
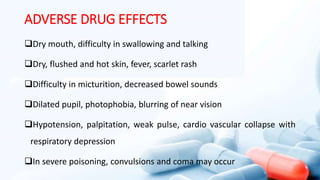
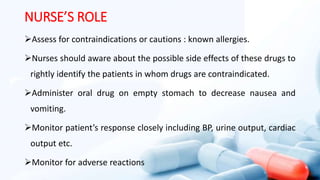
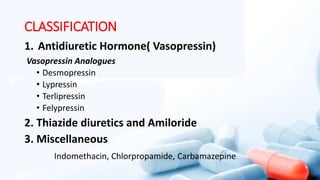
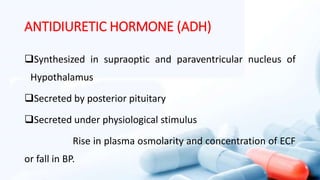
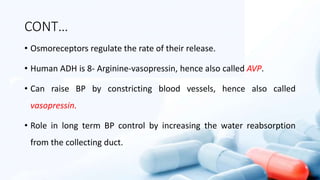
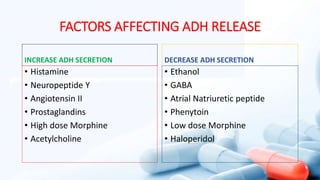
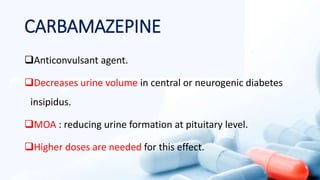
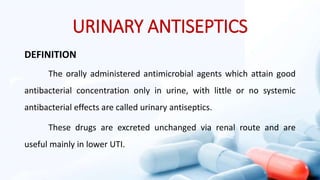
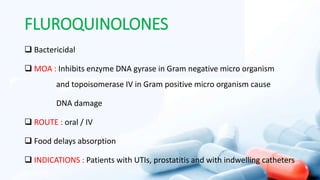
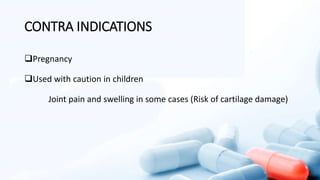
This document discusses various drugs used in the urinary system. It covers antidiuretic and antidiuretic hormone drugs that reduce urine volume, as well as urinary antiseptics like nitrofurantoin, fluoroquinolones, and cephalosporins. It also discusses cholinergic drugs that contract the bladder and ureter, and anticholinergic drugs that relax the bladder. Adverse effects and nursing roles are outlined.
















![CONT…
COTRIMOXAZOLE
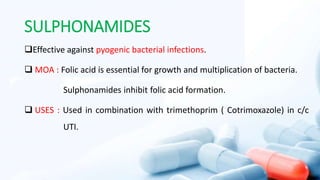
[Trimethoprim + Sulfamethoxazole ( Sulphonamide)]
80 mg + 400 mg tab : 2 BD for 2 days then 1 BD for 5-7 days.
160 mg + 800 mg tab (DS) : 1 BD for 5-7 days.
Pediatric dose
20 mg + 100 mg tab : for 5-7 days.
40mg + 200 mg per 5 ml suspension for 5-7 days.](https://image.slidesharecdn.com/pharmacology-urinarysystem-240214165706-a9b92c4e/85/pharmacology-Urinary-System-pptx-42-320.jpg)