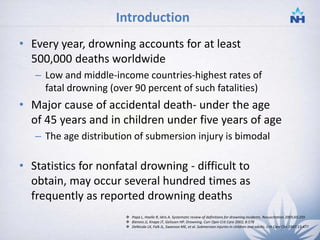
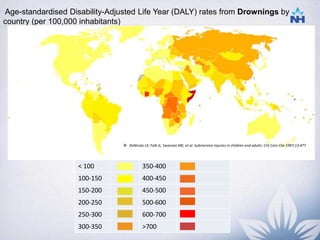
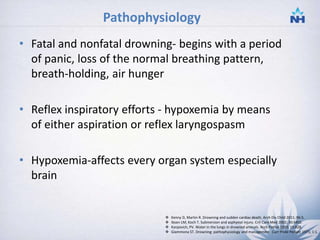
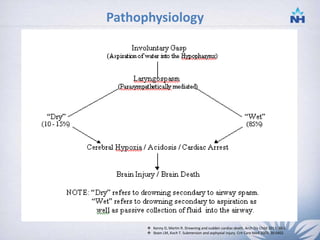
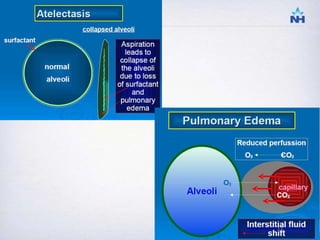
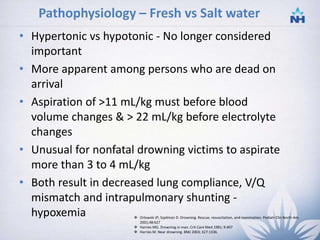
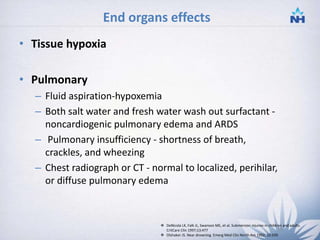
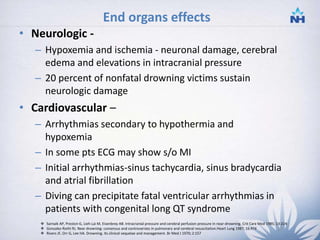
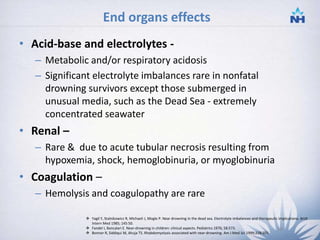
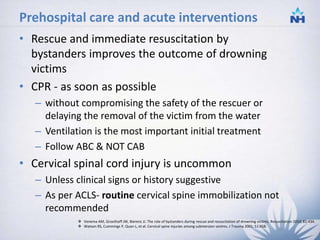
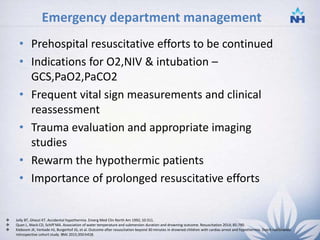
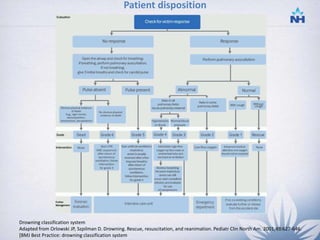
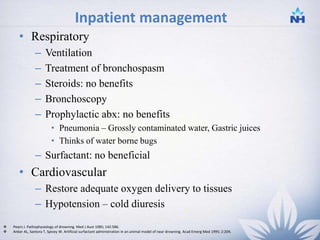
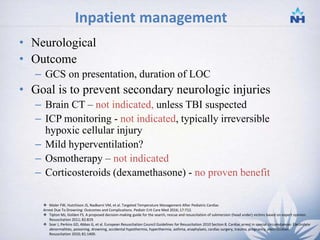
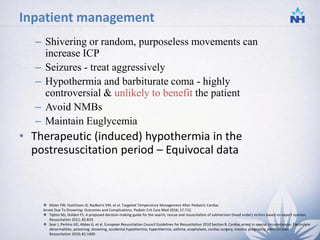
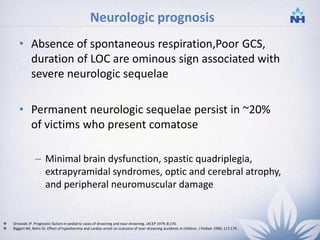
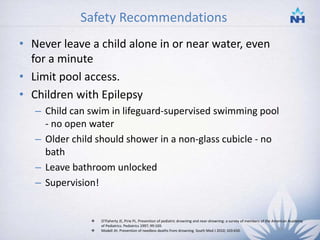
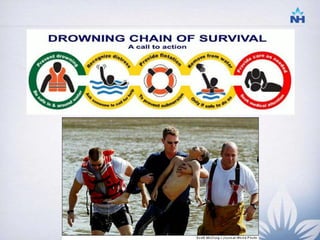
Drowning is a major public health issue worldwide, accounting for over 500,000 deaths per year. It is a leading cause of accidental death for those under age 45. The pathophysiology of drowning involves hypoxemia from aspiration of water into the lungs, which affects multiple organ systems. Management involves early rescue and CPR, with a focus on ventilation. In the hospital, patients may develop pulmonary edema, neurological impairment, or other end-organ effects and require monitoring and support. Standardizing definitions and reporting of drowning incidents can help improve outcomes.