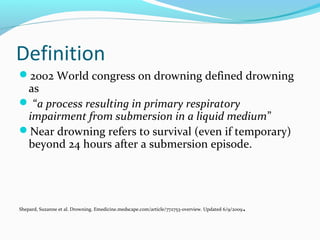
1. Drowning is defined as respiratory impairment from submersion in a liquid medium and is a major cause of accidental death, especially in children ages 1-14.
2. Management of drowning victims involves resuscitation, treatment of hypoxic-ischemic encephalopathy, and prevention of complications.
3. Prevention strategies focus on supervision during water activities, swimming lessons, CPR training, and safety measures around pools.

































![Connpatients, the Conn classification system may be
For other
classification system:
used as a guideline to quantify the extent of cerebral
hypoxia.
Category A – Alert
Category B - Blunted consciousness; admit and observe for
pulmonary compromise, which may result in hypoxemia
and worsen CNS injury
Category C - Comatose (C1 - decorticate, C2 - decerebrate,
and C3 - flaccid [worse prognosis than C1])](https://image.slidesharecdn.com/neardrowning-130315114423-phpapp01/85/Near-drowning-35-320.jpg)



