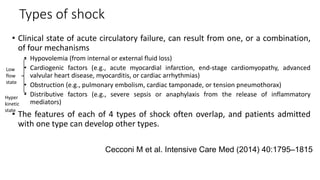
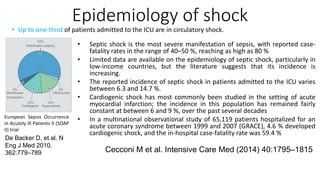
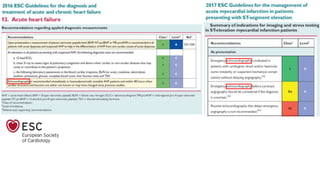
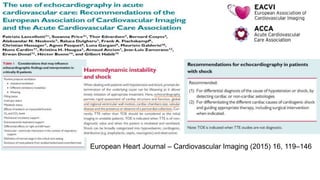
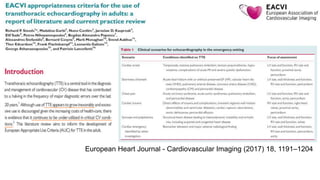
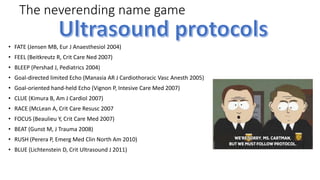
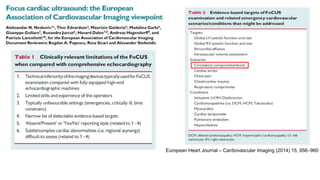
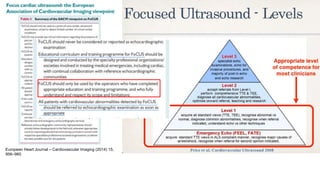
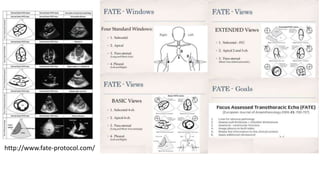
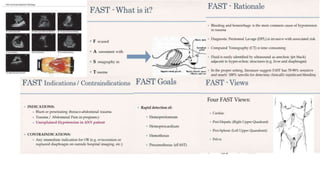
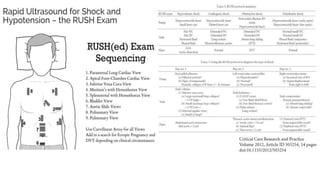
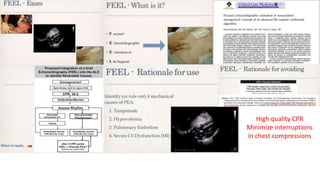
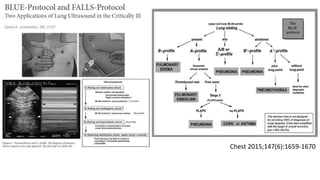
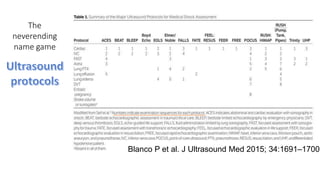
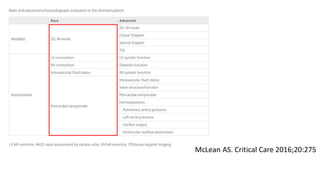
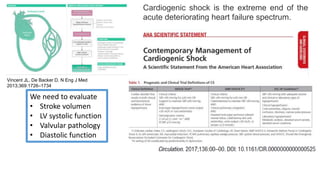
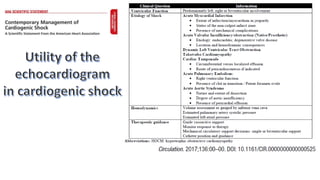
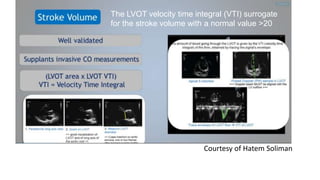
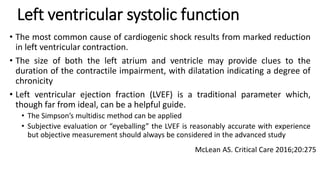
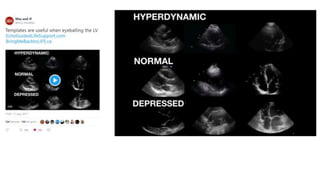
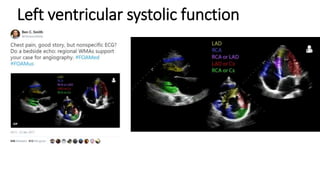
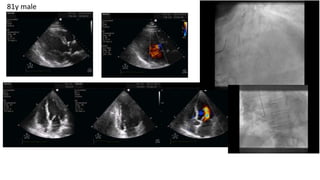
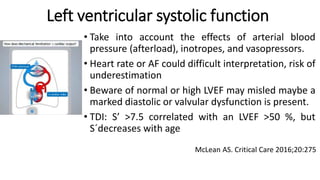
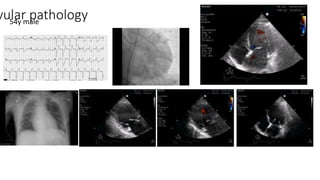
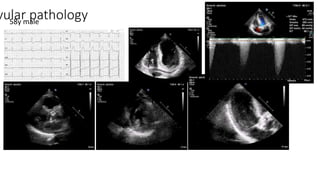
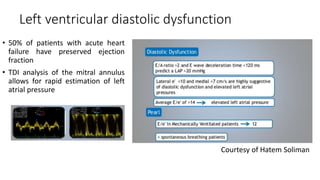
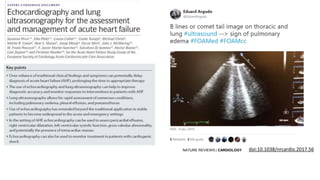
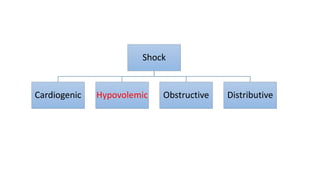
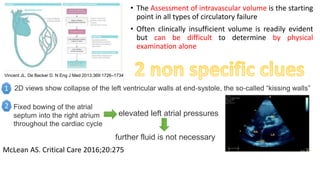
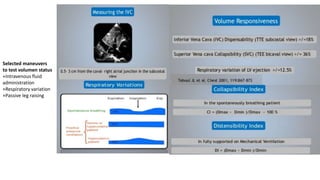
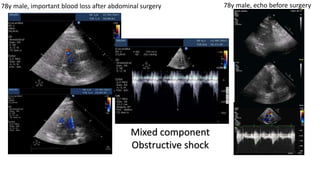
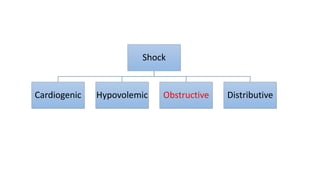
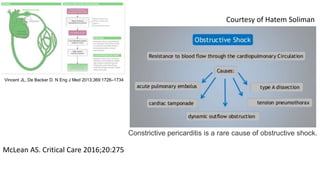
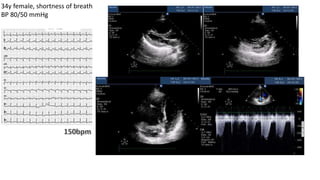
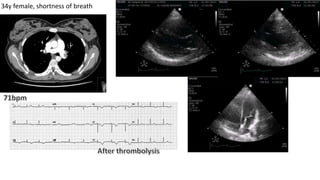
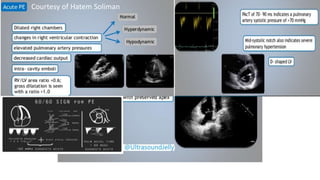
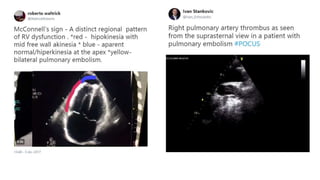
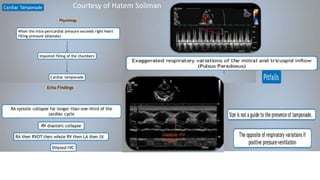
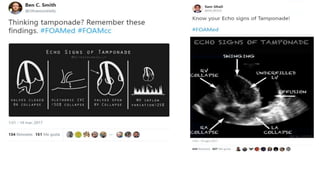
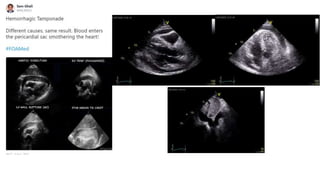
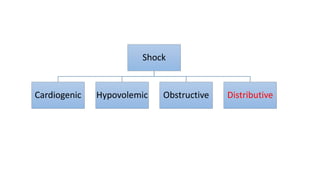
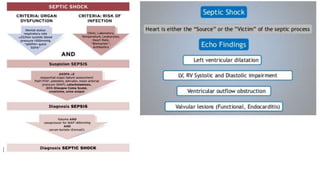
This presentation discusses how to evaluate shock using echocardiography. It defines shock and describes the main types: hypovolemic, cardiogenic, obstructive, and distributive. Guidelines recommend using echo to evaluate shock. The presentation reviews how to assess left ventricular systolic function, volume status, valvular pathology, and diastolic function. It provides examples of using echo to diagnose specific causes of shock like sepsis, myocardial infarction, pulmonary embolism, and tamponade. The key messages are that echo is very useful for diagnosing and managing shock, and training in point-of-care ultrasound is important.


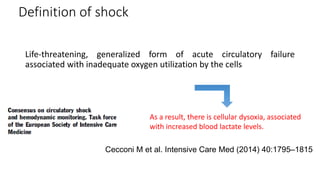
![Definition of shock
Diagnosis based on a combination of clinical, hemodynamic and biochemical signs
• Clinical signs of shock typically include.-
• Arterial Hypotension (although this is not always present),
• Signs of altered tissue perfusion, visualized through the 3 ‘windows’ of the body
• Peripheral window (skin that is cold, clammy & blue, pale or discolored)
• Renal window (decreased urine output: <0.5 mL/kg/h)
• Neurologic window (altered mental characterized by obtundation,
disorientation & confusion)
• Presence of Arterial Hypotension [defined as systolic blood pressure of <90 mmHg, or
mean arterial pressure (MAP) of <65 mmHg, or a decrease of ≥40 mmHg from baseline],
while commonly present, should not be required to define shock
• Lactate levels are typically >2 mEq/L (or mmol/L) in shock states
Cecconi M et al. Intensive Care Med (2014) 40:1795–1815](https://image.slidesharecdn.com/howtoevaluateshockbyecho-copia-171206023827/85/How-to-evaluate-shock-by-echo-6-320.jpg)