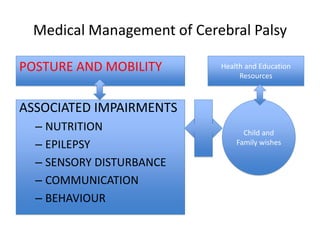
This document discusses cerebral palsy (CP), including its classification, epidemiology, and medical management. Some key points:
1) CP affects 2-3 per 1000 children and is the most common cause of physical disability in childhood. There has been ongoing debate around its definition and classification.
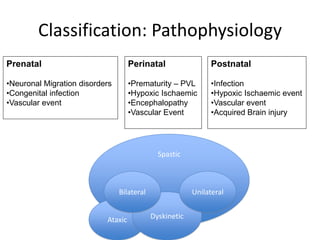
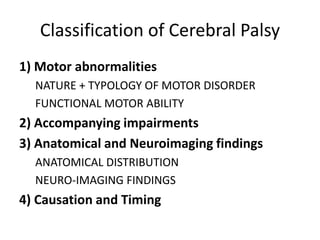
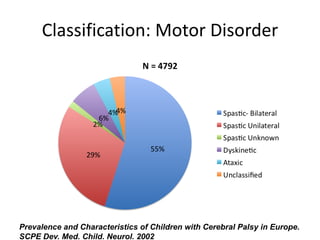
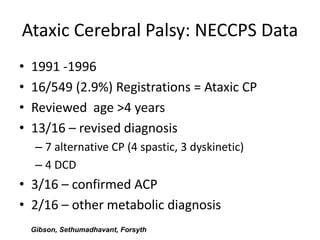
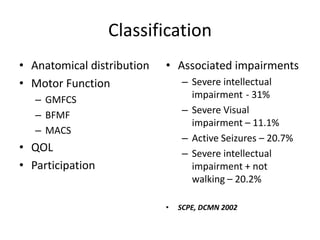
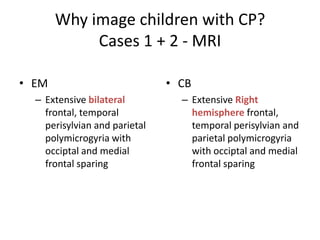
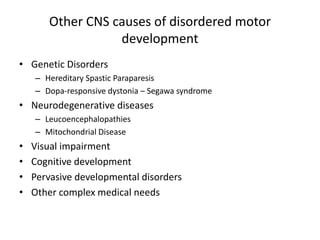
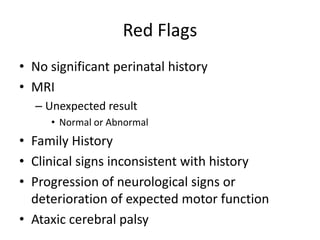
2) CP is classified based on the type of motor disorder (spastic, dyskinetic, ataxic, or mixed), functional motor ability, accompanying impairments, and suspected causation/timing.
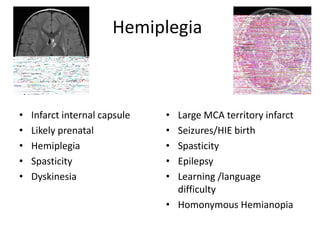
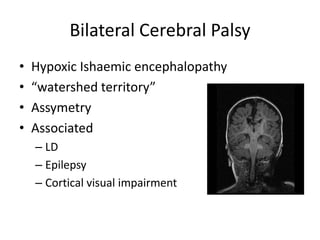
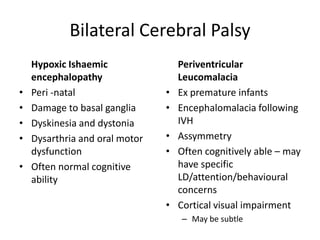
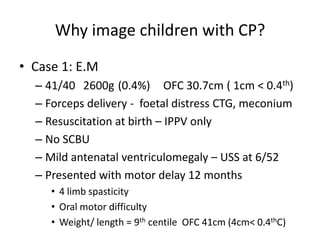
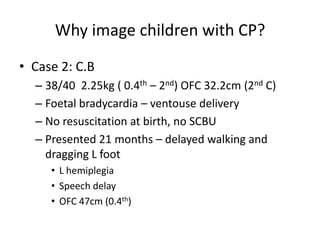
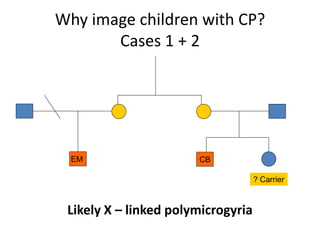
3) Risk factors for CP include prematurity, hypoxic-ischemic encephalopathy, infection, and vascular events during fetal or infant brain development. Imaging can help determine the anatomical distribution and nature