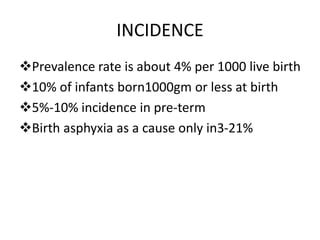
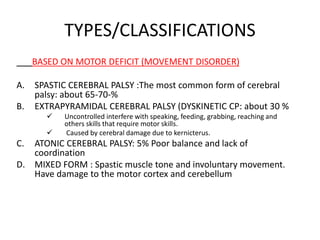
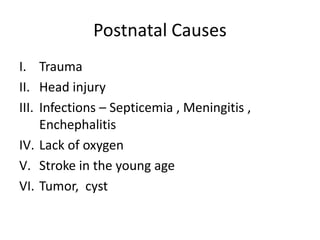
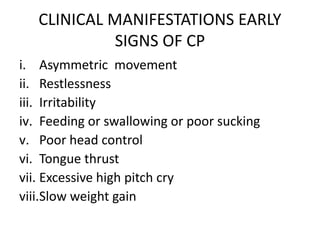
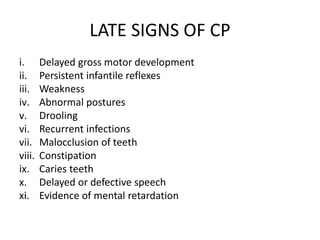
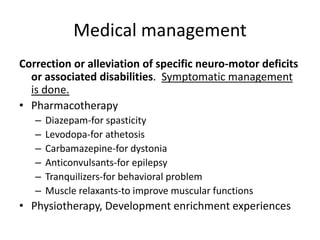
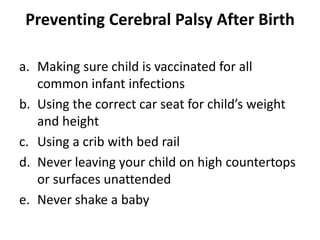
This document discusses cerebral palsy (CP), including its definition, types, causes, signs and symptoms, and treatment/management approaches. CP is a group of disorders that impair movement and posture due to non-progressive brain damage early in development. It has a prevalence of about 4 per 1,000 live births. The main types are spastic, dyskinetic, atonic, and mixed. Causes include genetic factors, issues with the mother or pregnancy, perinatal complications, postnatal infections or injuries, and lack of oxygen. Signs vary depending on severity but may include abnormal movements, poor head control, feeding difficulties, and developmental delays. Treatment aims to manage symptoms, prevent complications, and support development