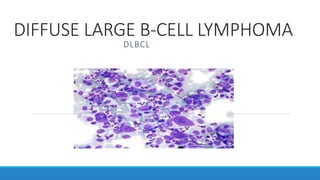
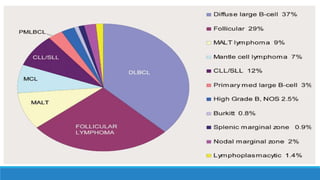
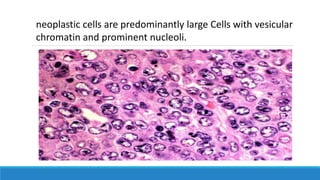
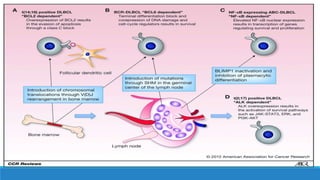
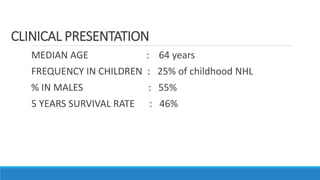
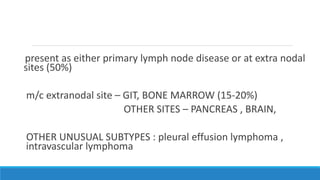
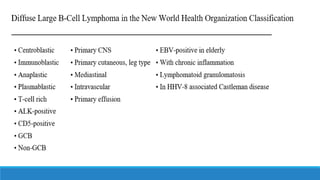
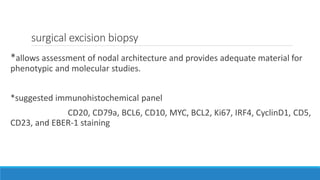
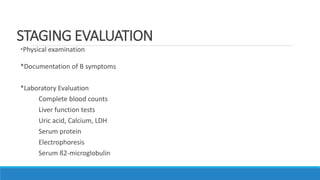
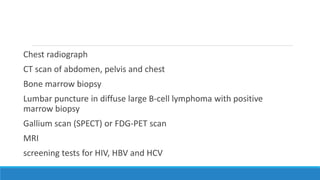
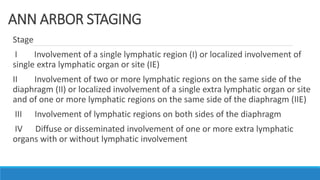
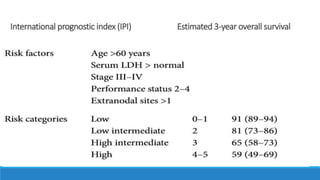
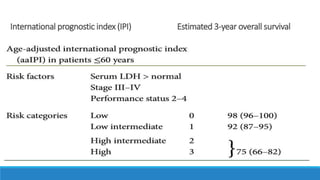
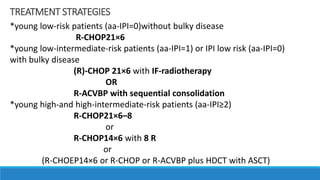
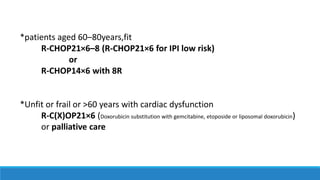
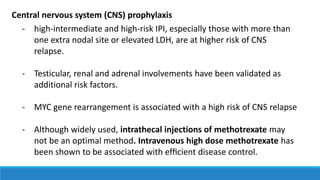
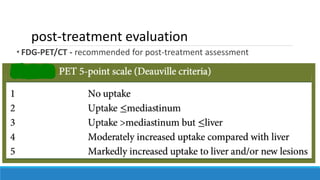
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, making up 30-40% of cases. DLBCL is an aggressive or intermediate-grade lymphoma characterized by large malignant B cells. Risk factors include family history of lymphoma, autoimmune disease, HIV/HCV infection, and high body mass index. Treatment involves chemotherapy such as R-CHOP along with radiation or stem cell transplant depending on risk factors and age. Prognosis depends on factors like stage and the international prognostic index, with 5-year survival rates around 46% on average.