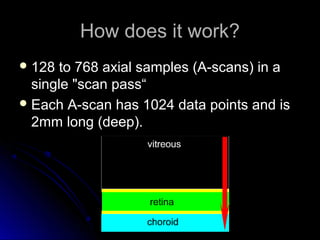
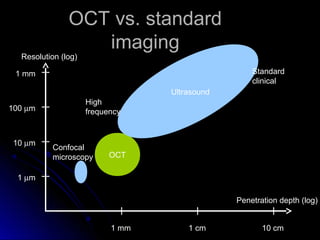
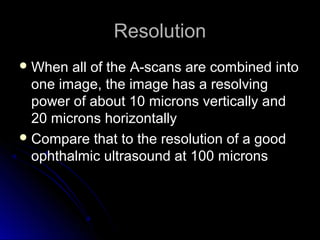
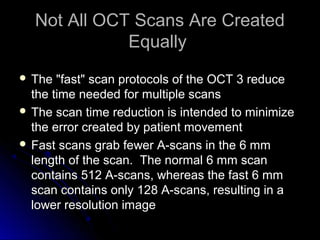
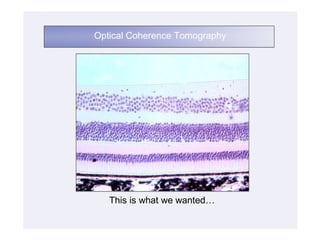
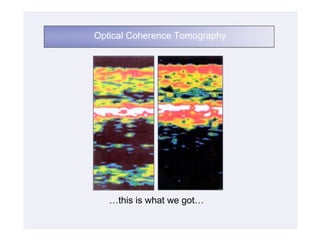
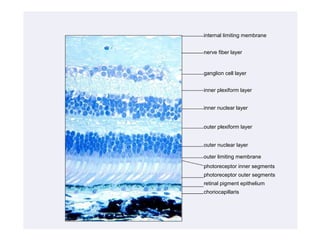
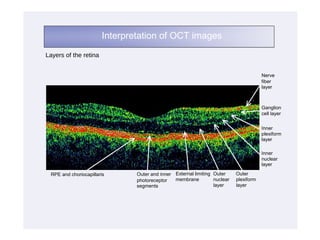
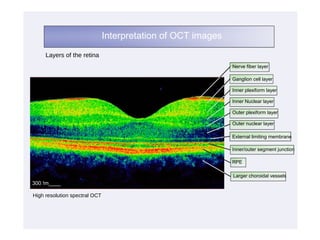
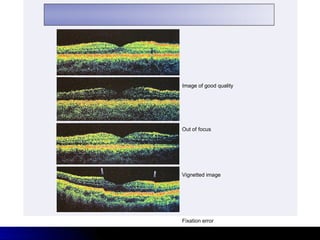
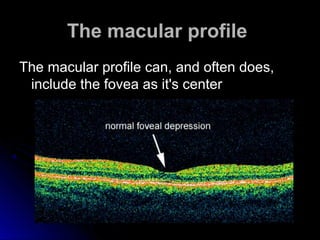
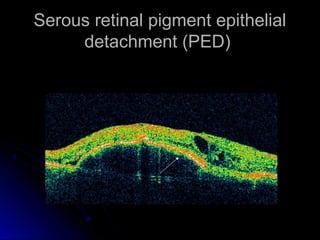
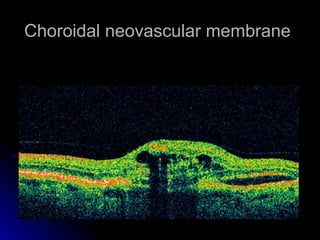
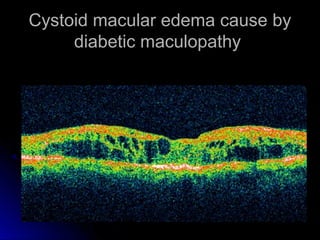
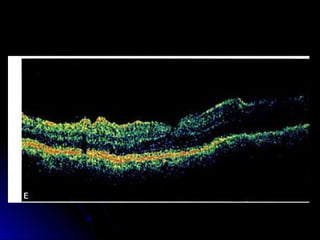
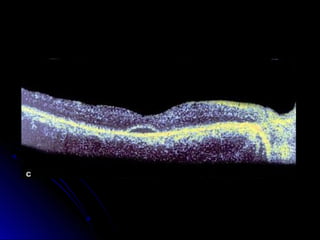
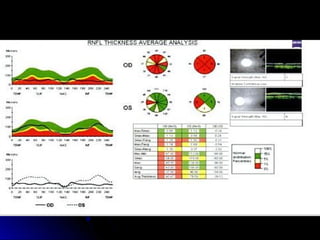
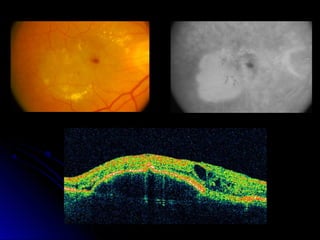
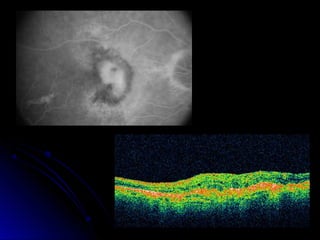
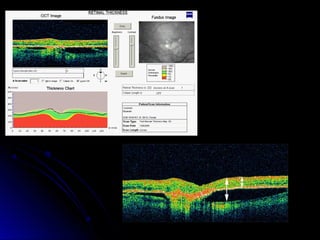
Optical coherence tomography (OCT) is a non-invasive imaging technique that examines living tissue using low coherence radiation. OCT allows for both qualitative and quantitative analysis of the retina. Qualitatively, OCT can describe retinal structures and anomalies. Quantitatively, OCT can measure retinal thickness and nerve fiber layer thickness. OCT works by capturing 128 to 768 axial scans in a single pass, with each scan containing 1024 data points over a 2mm depth. OCT has higher resolution and penetration depth than standard clinical imaging.