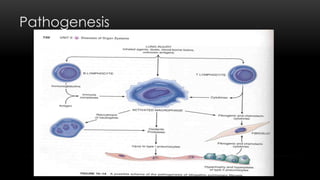
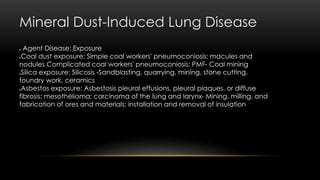
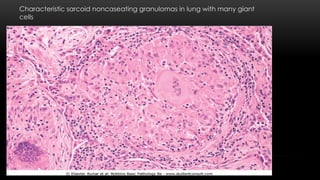
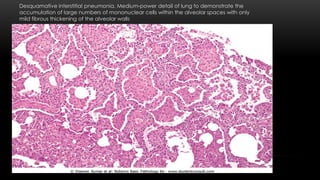
This document discusses diffuse interstitial (infiltrative, restrictive) lung diseases. It defines them as heterogeneous disorders characterized by diffuse chronic involvement of pulmonary connective tissue. The major categories discussed include fibrosing, granulomatous, eosinophilic, and smoking-related diseases. Specific conditions like idiopathic pulmonary fibrosis, sarcoidosis, and pneumoconiosis are examined in terms of their pathogenesis, morphology, and clinical course.