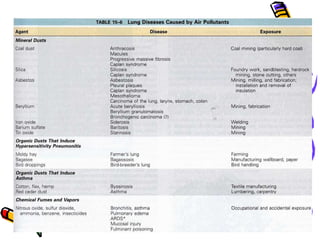
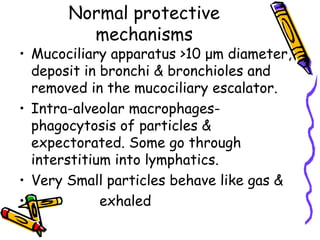
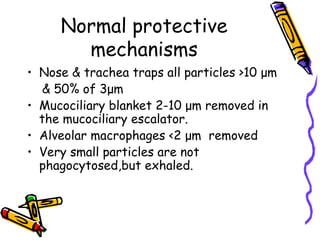
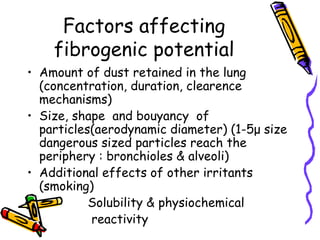
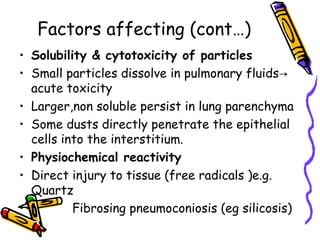
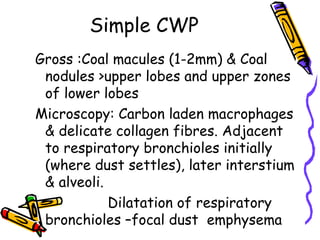
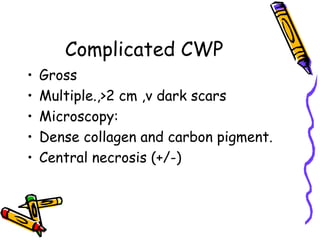
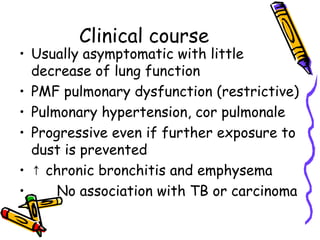
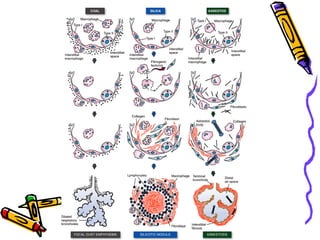
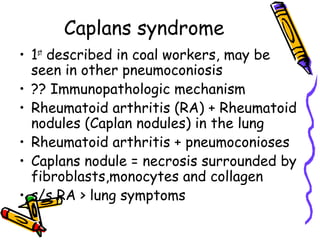
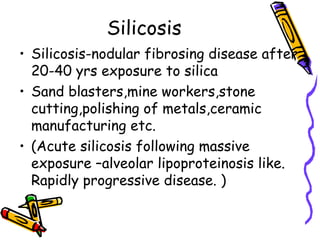
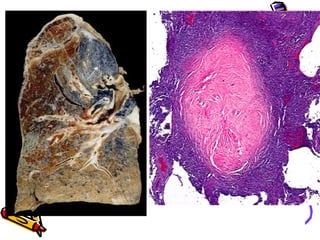
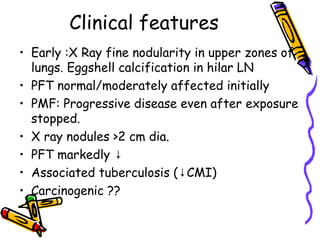
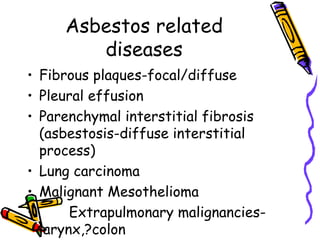
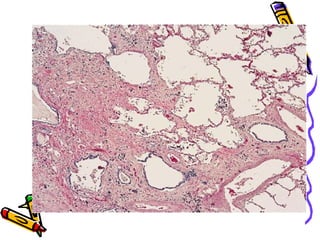
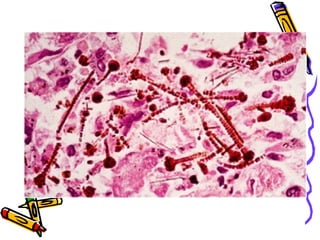
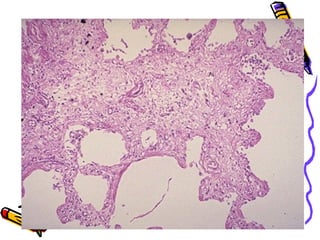
This document summarizes pneumoconiosis, which are non-cancerous lung diseases caused by inhaling mineral or metallic dusts. It discusses the definition, types based on causative agents like silica and coal, normal lung protective mechanisms, factors affecting disease development, pathogenesis, clinical features of specific types like coal workers' pneumoconiosis and silicosis, and prevention. Pneumoconiosis are important to diagnose as occupational lung diseases.