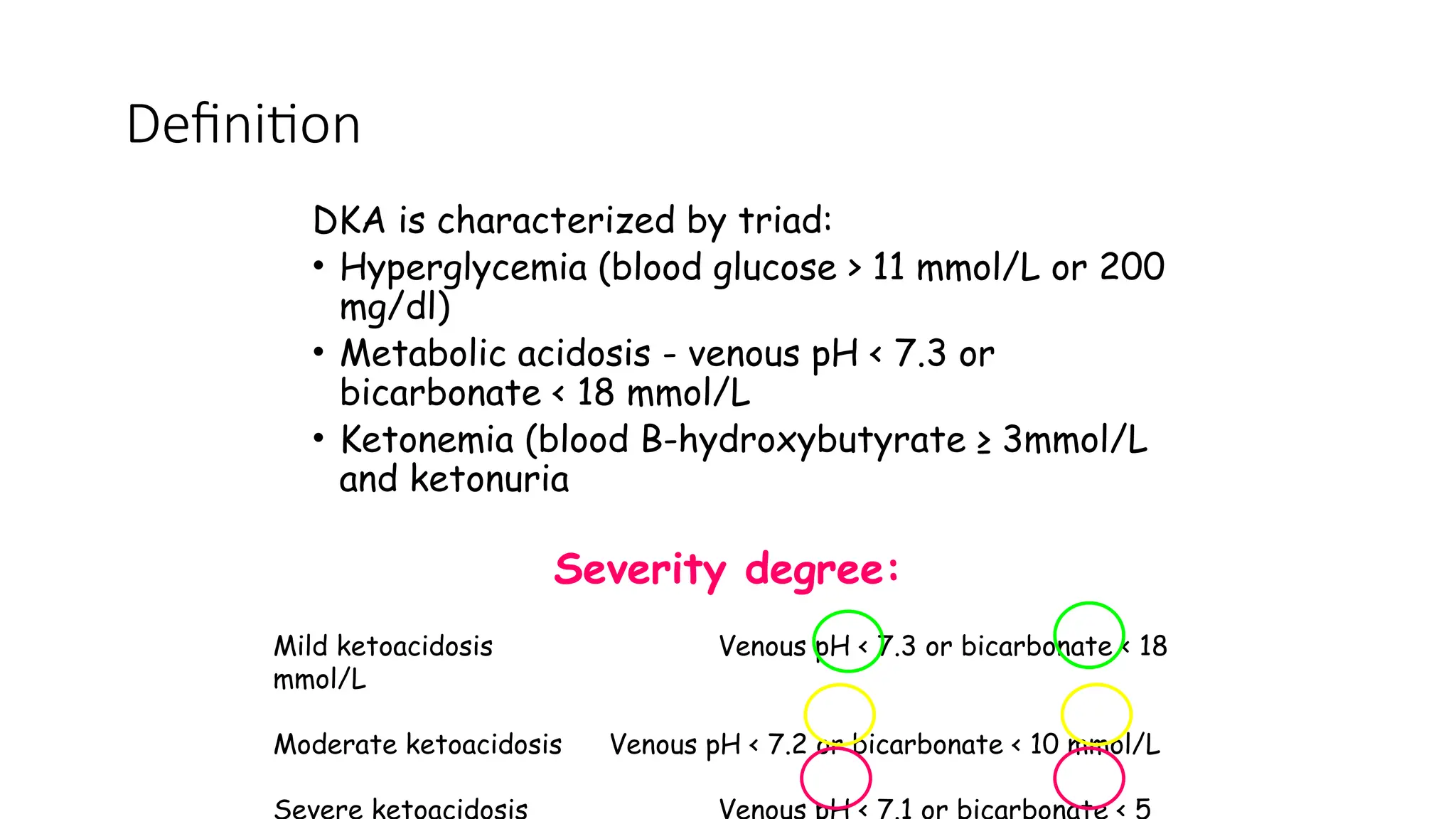
Diabetic ketoacidosis (DKA) is a critical condition commonly presented in children with diabetes, characterized by hyperglycemia, metabolic acidosis, and ketonemia. The lecture outlines the definitions, diagnostic criteria, pathophysiology, and treatment protocols for DKA, emphasizing the importance of early recognition and management to reduce mortality rates. Preventive measures against recurrence include addressing insulin omission and managing psychosocial factors that contribute to non-compliance.