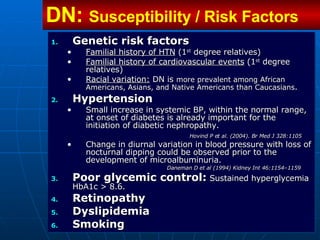
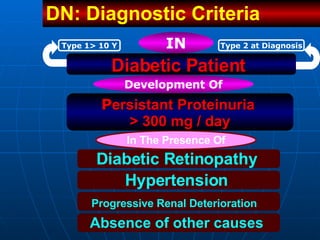
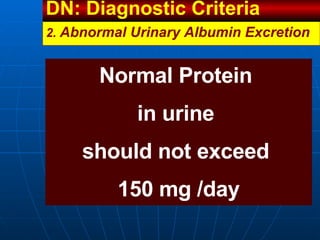
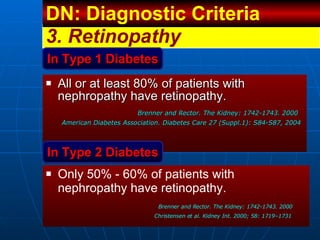
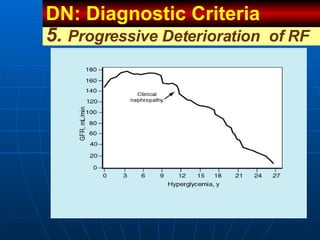
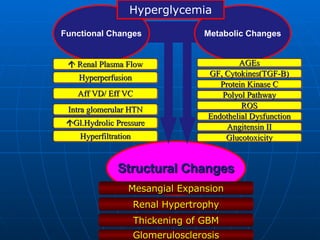
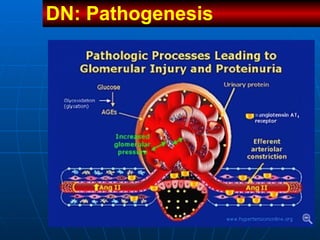
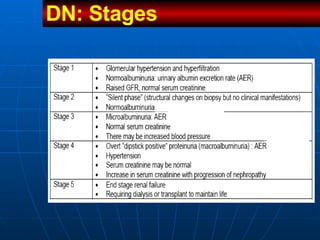
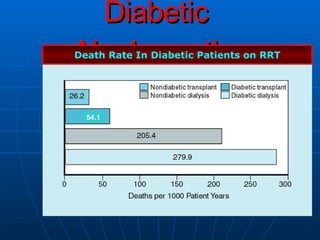
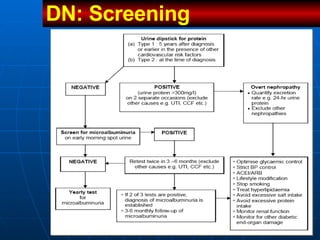
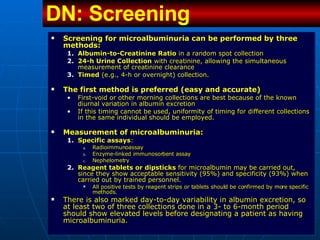
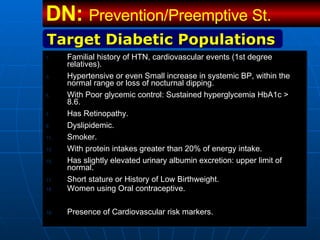
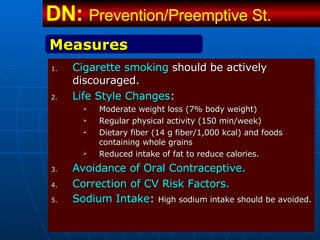
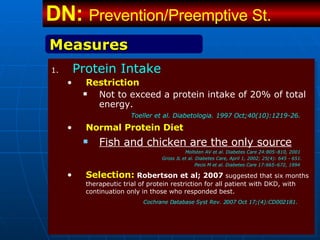
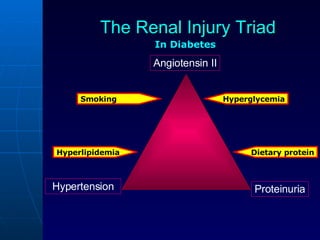
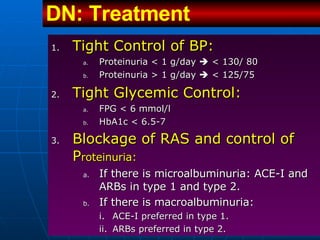
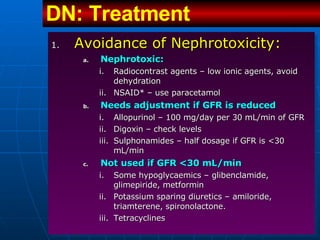
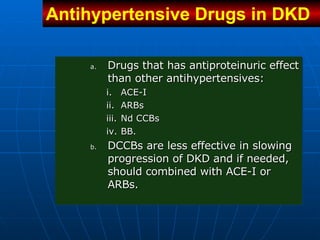
This document discusses diabetic nephropathy, including its causes, risk factors, stages, diagnosis, progression, and treatment strategies. It notes that diabetic nephropathy is a major complication of diabetes and a leading cause of end-stage renal disease. Key points include that strict control of blood pressure, blood glucose, diet, and lifestyle factors can help prevent or slow the progression of kidney damage caused by diabetes.