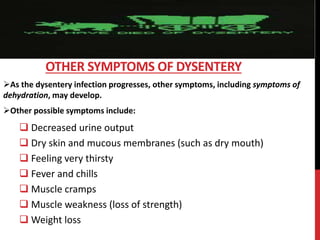
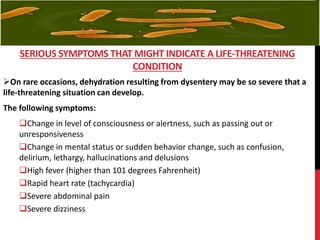
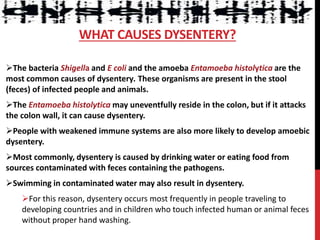
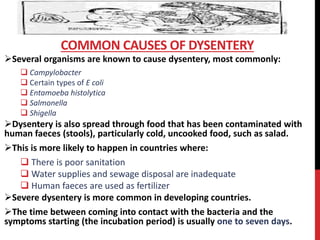
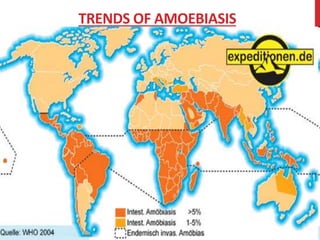
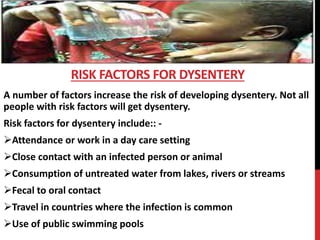
Dysentery is a gastrointestinal disease characterized by abdominal pain and bloody diarrhea caused by bacteria, viruses or parasites. Common symptoms include abdominal cramps, bloody stool and fever. It is usually spread through contaminated food or water. Treatment involves antibiotics, rehydration and rest. Prevention focuses on proper handwashing and drinking purified water. Dysentery remains a major public health problem, especially in developing countries, where it claims many lives each year.