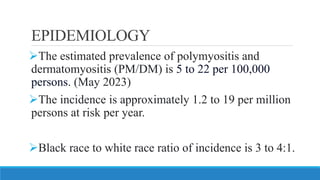
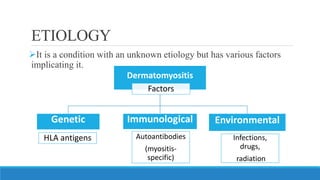
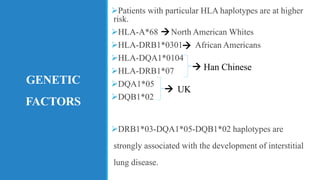
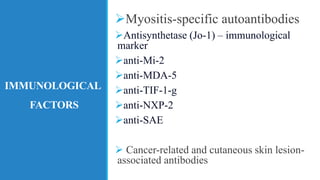
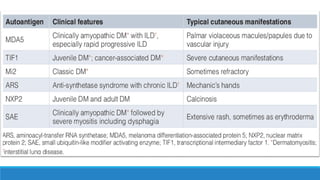
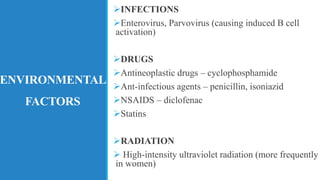
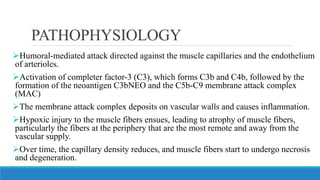
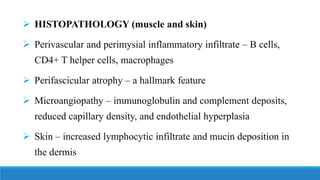
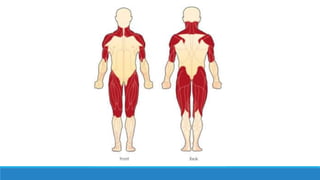
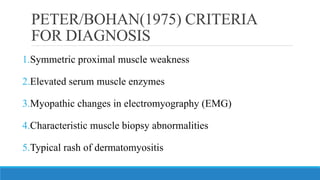
Dermatomyositis is a rare autoimmune disease characterized by muscle weakness and a skin rash. It affects the skin, muscles, lungs, heart, and gastrointestinal system. Genetic and environmental factors may play a role in its development. Diagnosis involves assessing muscle weakness, increased muscle enzymes, skin changes like a heliotrope rash or Gottron's papules, and muscle biopsy. Treatment focuses on immunosuppressants, corticosteroids, immunoglobulins, and physical therapy to maintain muscle strength and function.