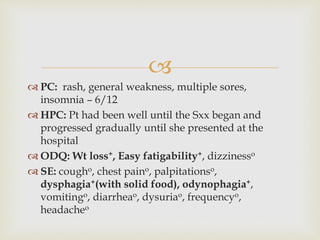
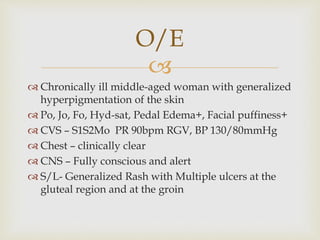
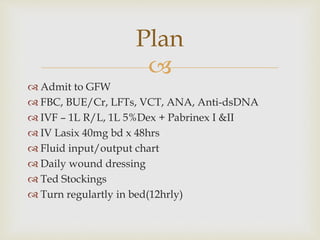
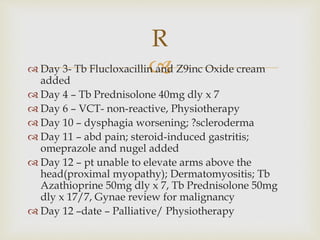
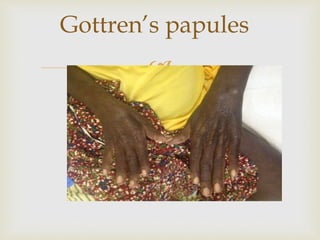
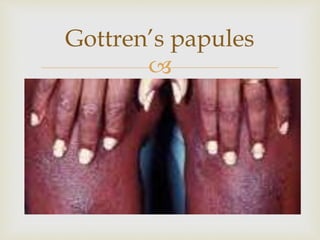
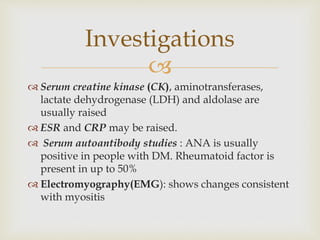
A middle-aged woman presented with generalized weakness, rashes, and sores. On examination, she had hyperpigmentation, edema, and rashes on her buttocks and groin. Tests found elevated muscle enzymes. She was diagnosed with dermatomyositis and admitted for IV fluids and steroids. Her symptoms worsened, and she developed difficulty raising her arms, confirming the diagnosis of dermatomyositis. She was started on immunosuppressants and referred for palliative care.