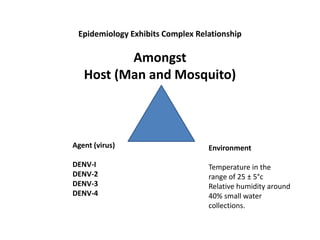
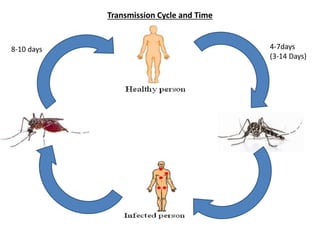
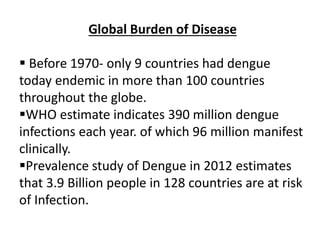
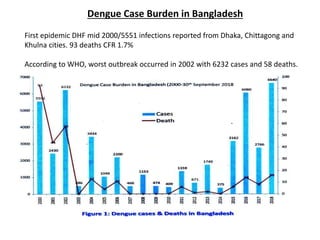
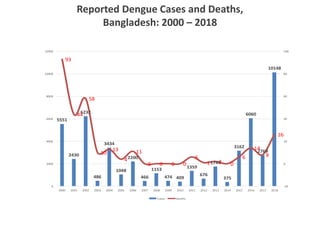
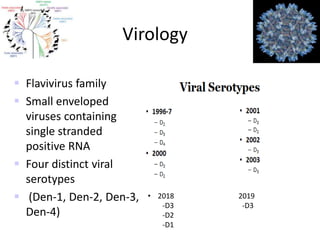
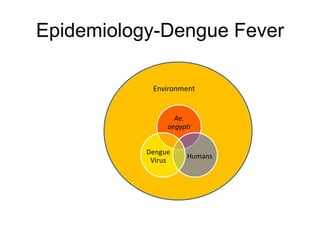
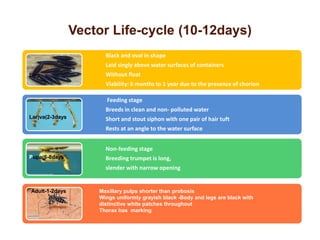
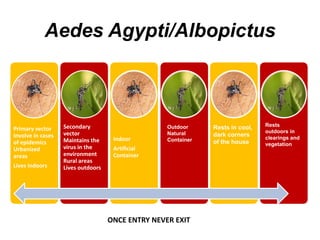
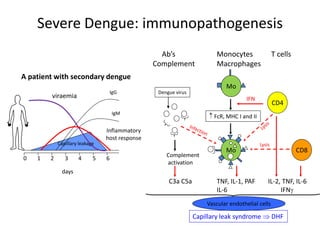
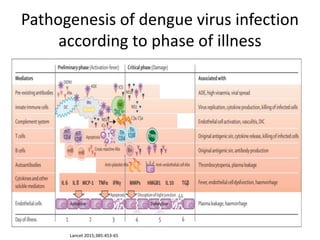
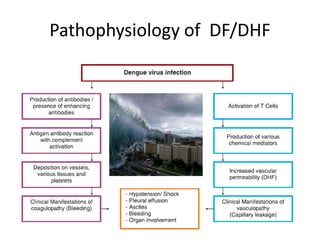
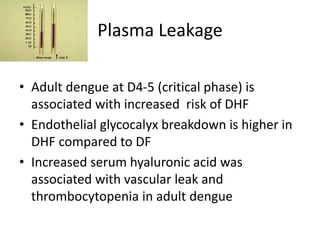
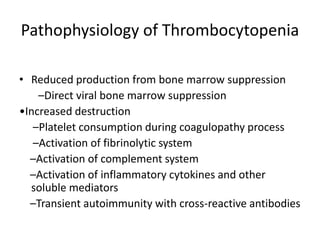
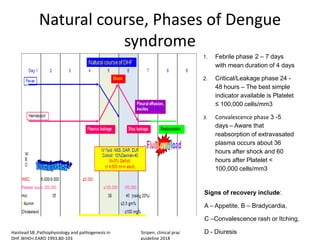
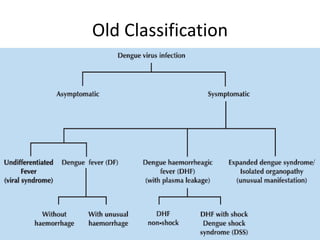
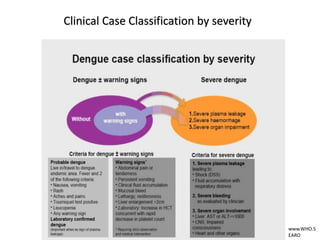
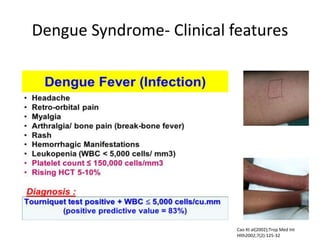
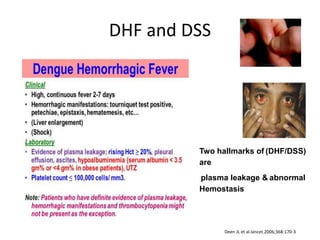
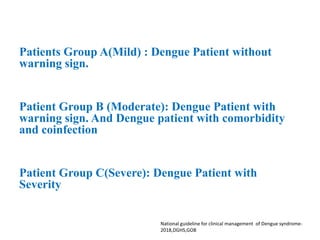
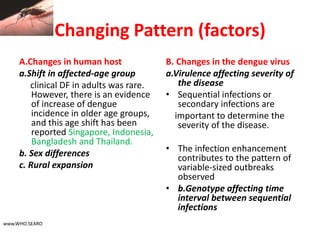
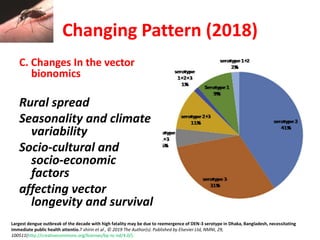
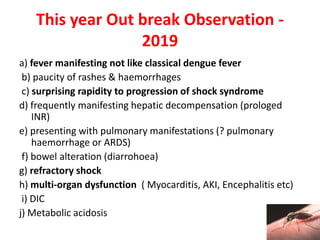
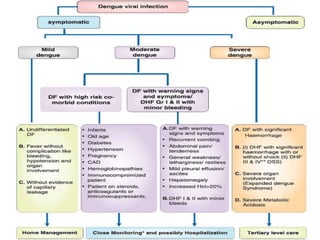
Dr. Shahadad Hossain presented an update on dengue management. Dengue is a systemic viral infection transmitted through Aedes mosquitoes. While the disease manifestations are complex, treatment is simple and effective if cases are detected early through organized processes like classification and referral when needed. Dengue epidemiology involves interactions between the virus, human hosts, mosquito vectors, and environmental factors like temperature and humidity. Four distinct dengue virus serotypes exist. The global burden of dengue is high and increasing, with 390 million estimated annual infections. Bangladesh has experienced several major dengue outbreaks, with the largest in 2002. Proper management requires understanding the virus, vector, transmission cycle, immunopathogenesis involving antibody-dependent enhancement



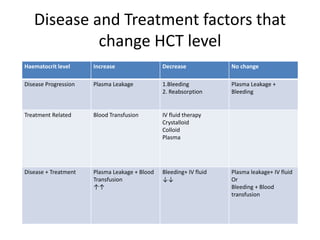
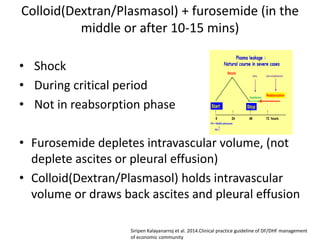
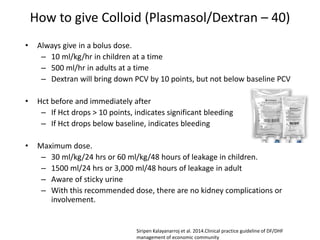
![Indications for using Colloid [(10%
Dextran-40 in NSS)/Plasmasol/Human
albumin]
• Signs of fluid overload
• Dyspnea, tachypnea, puffy eyelids,
tense/distended abdomen
• Positive lung signs: crepitation, rhonchi,
wheezing
• Persistent high Hct, 25 - 30%
hemoconcentration for > 4-8 hours.
Siripen Kalayanarroj et al. 2014.Clinical practice guideline of DF/DHF management
of economic community](https://image.slidesharecdn.com/denguein2019finaldkd-200103132941/85/dengue-fever-management-91-320.jpg)