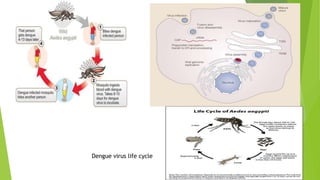
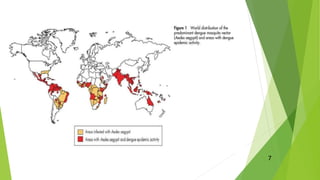
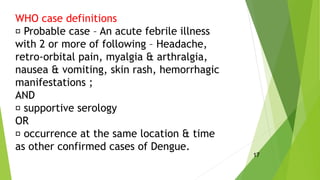
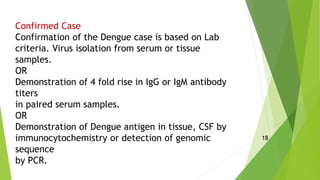
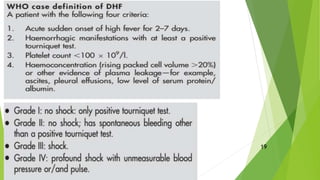
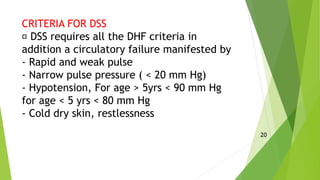
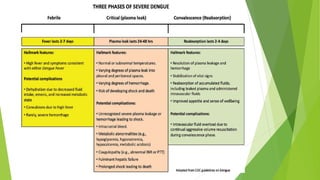
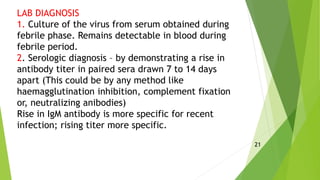
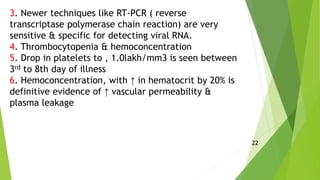
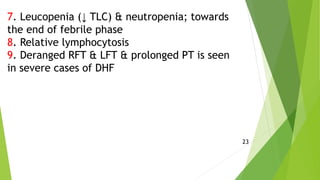
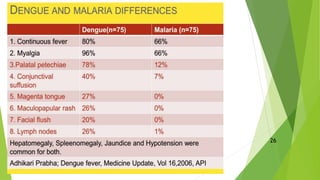
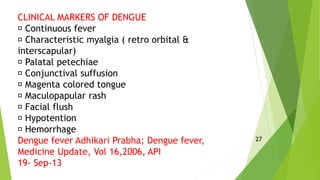
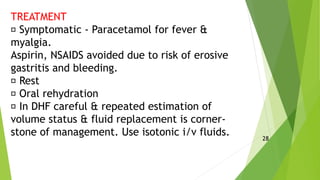
Dengue is a mosquito-borne viral disease caused by the dengue virus. It is transmitted by the Aedes aegypti mosquito. There are four different serotypes of the virus that cause lifelong immunity after infection. Dengue presents as a sudden onset of fever, headache, muscle and joint pains. A transient rash and bleeding manifestations may occur. Dengue hemorrhagic fever is defined as fever with bleeding and low platelets. Dengue shock syndrome involves circulatory failure in addition to DHF criteria and has high mortality. There is no vaccine available though control of mosquito breeding is key to prevention. Treatment involves symptom relief and fluid management to prevent shock.