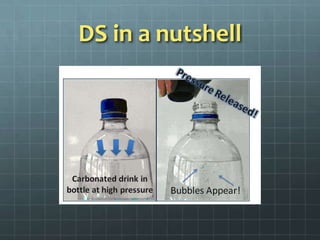
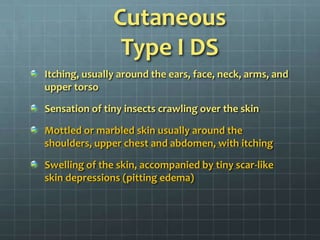
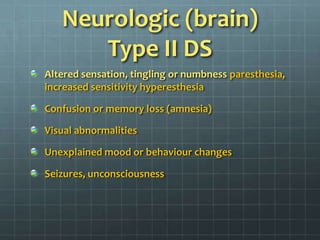
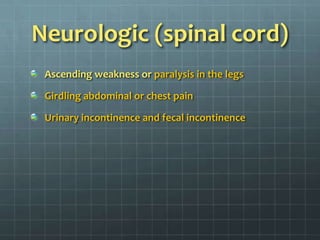
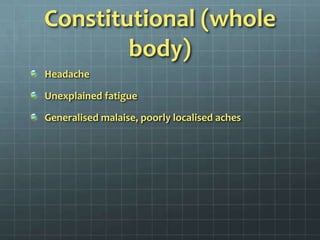
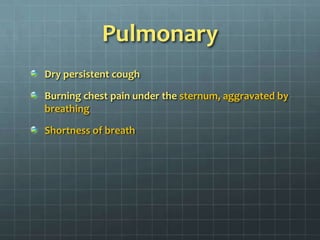
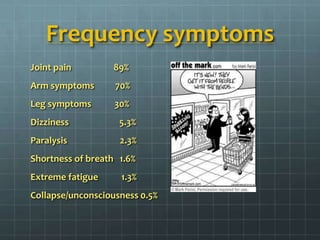
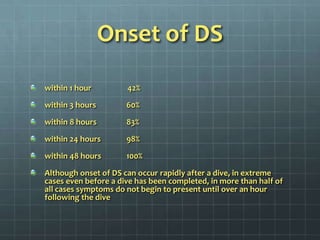
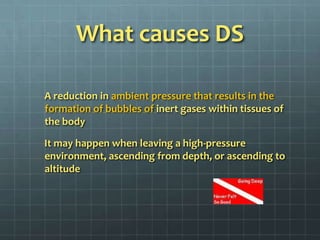
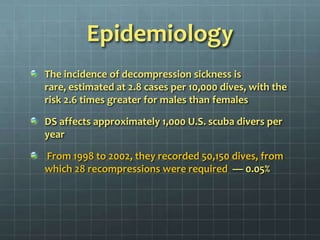
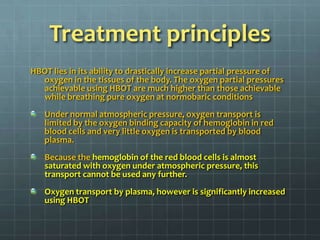
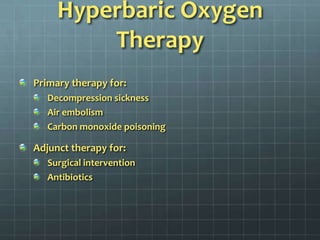
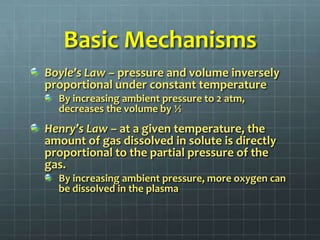
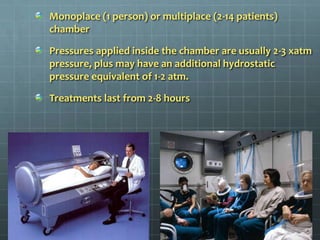
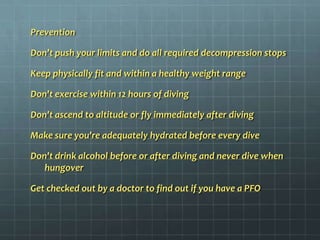
Decompression sickness (DS), also known as "the bends", can occur in scuba divers and others exposed to significant changes in atmospheric pressure. It is caused by nitrogen bubbles forming in the body if the pressure drops too quickly. DS is classified as type I or type II depending on whether skin/joints or other organs are affected. Common symptoms include joint pain, rashes, dizziness and paralysis. Treatment involves oxygen therapy followed by recompression in a hyperbaric chamber to dissolve the bubbles. Risk factors include ascent rate, depth, repetitive dives and individual traits like age and body type. Prevention focuses on following safe ascent procedures and dive tables to avoid dangerous pressure changes.