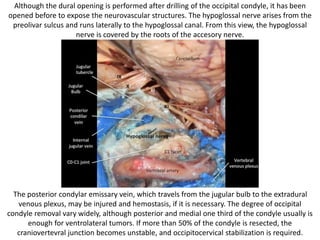
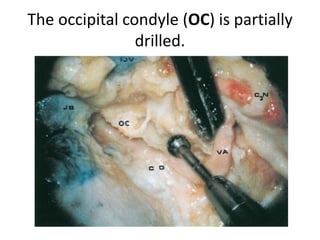
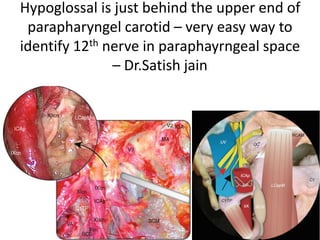
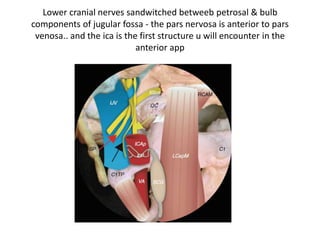
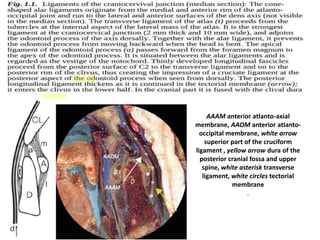
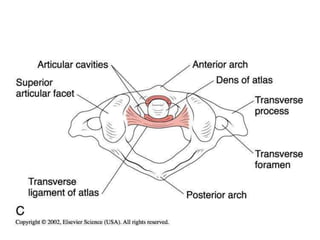
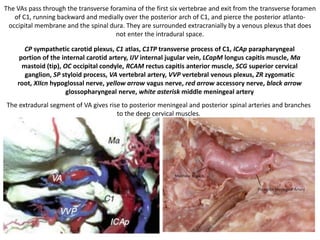
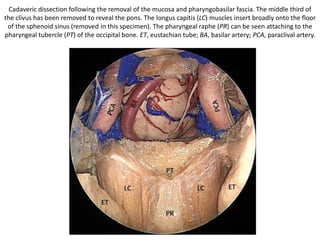
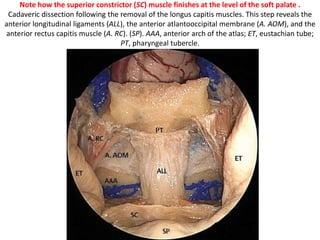
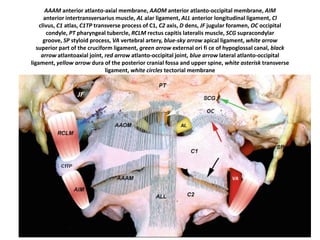
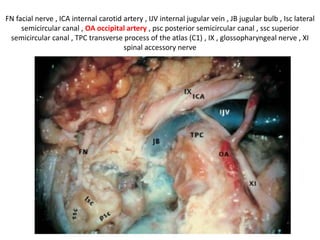
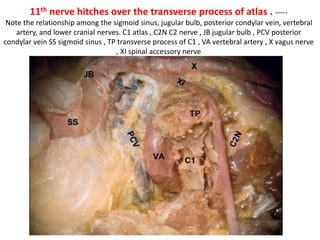
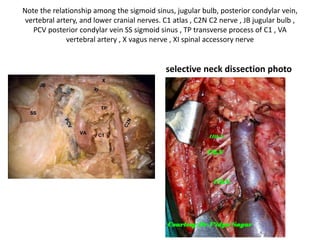
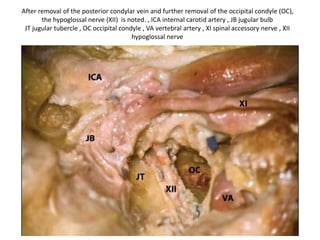
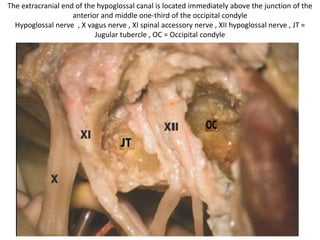
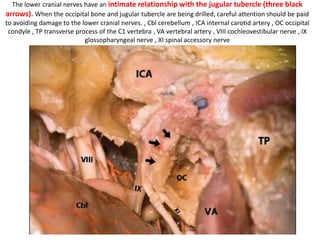
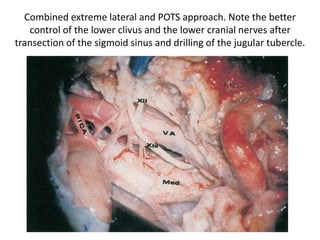
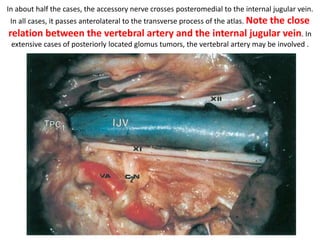
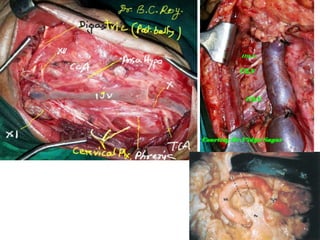
1. The document provides detailed anatomical descriptions and diagrams of the craniovertebral junction and foramen magnum region. It describes key landmarks such as the hypoglossal canal, jugular tubercle, pharyngeal tubercle, and their relationships to surrounding structures.
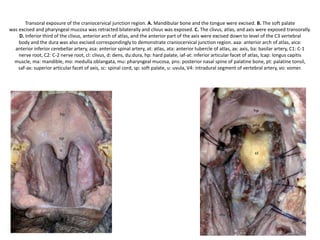
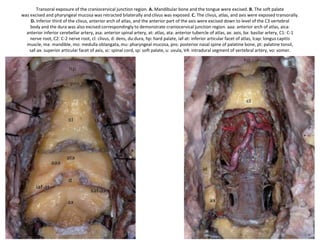
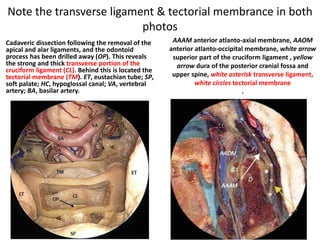
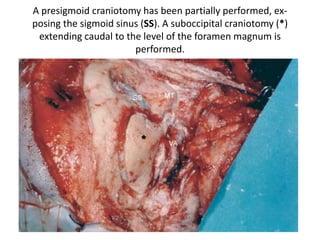
2. Surgical approaches to this region are discussed, including a transoral approach where the soft palate and portions of bone can be removed to fully expose the clivus, atlas, and axis.
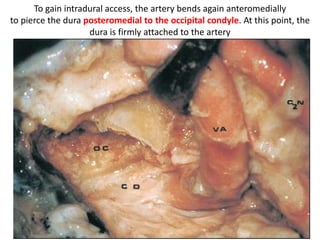
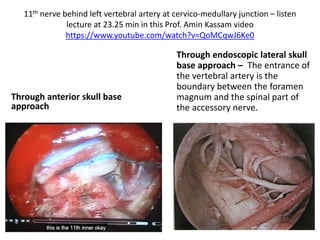
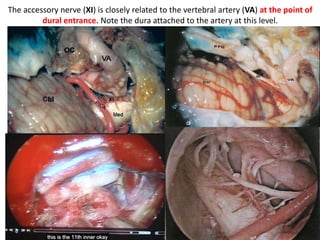
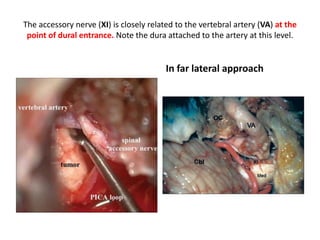
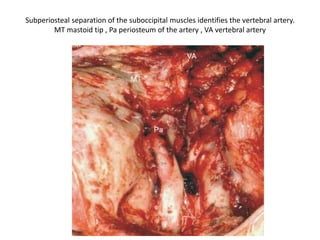
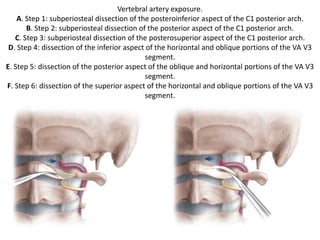
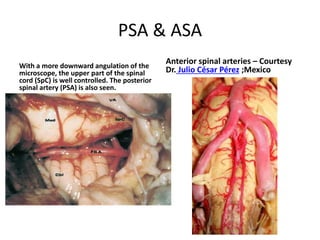
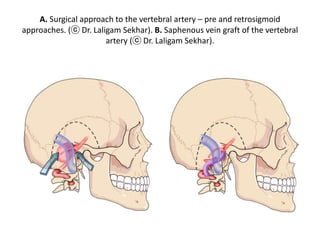
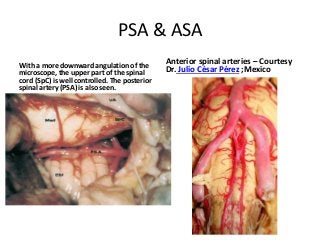
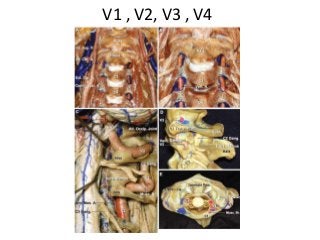
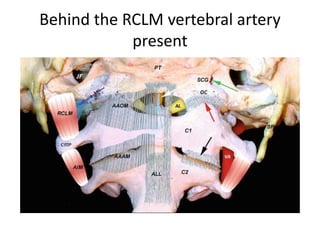
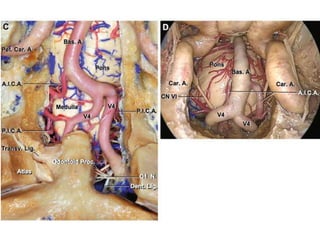
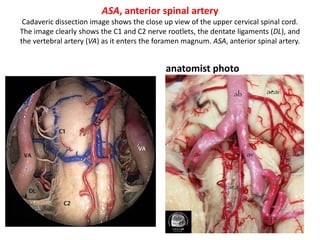
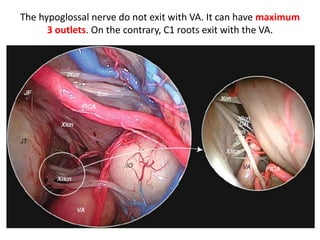
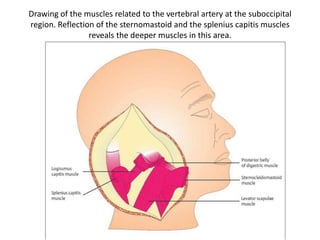
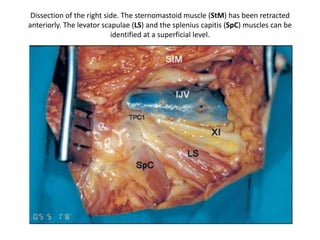
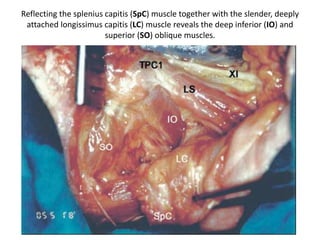
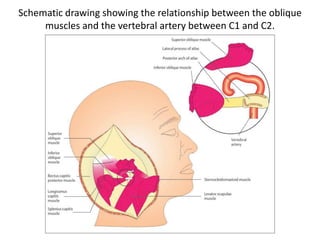
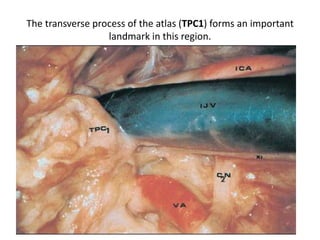
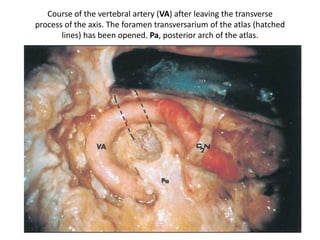
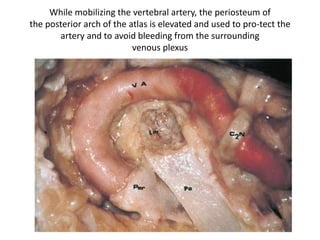
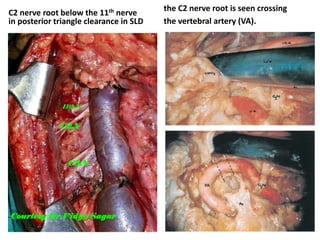
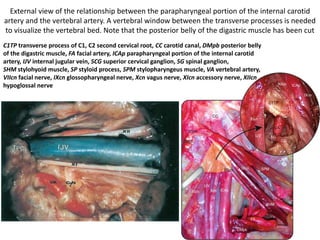
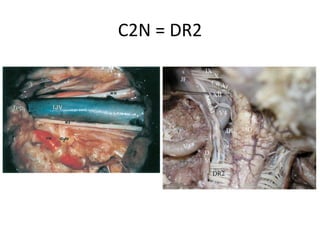
3. Important vascular structures like the vertebral artery and its relation to nearby muscles are depicted. The document serves as a comprehensive reference for the intricate anatomy of the lower skull base.

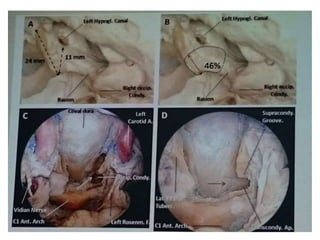
![1. The HC divides the condylar region into the tubercular compartment
(superior) and the condylar compartment (inferior).
Tubercular compartment contains LPT lateral pharyngeal tubercle, PT
pharyngeal tubercle,
2. The SCG [Supracondylar groove] represents a reliable landmark for hypoglossal
canal (HC) identification (red arrow) (Morera et al. 2010 ) .](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-5-320.jpg)
![The tubercular compartment corresponds to the Jugular tubercle ( JT )
Line along the lateral pharyngeal tubercle [ LPT ] passes through
Jugular tubercle [ JT ] – so when you are drilling LPT in anterior skull
base you will land up on JT .
LPT lateral pharyngeal tubercle, OC
occipital condyle, PT pharyngeal
tubercle, SCG supracondylar groove
Jugular tubercle ( JT )](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-6-320.jpg)
![Line along the lateral pharyngeal tubercle [ LPT ] passes through Jugular tubercle [ JT
] – so when you are drilling LPT in anterior skull base you will land up on JT .
Red rings = hypoglossal canals , yellow
ring = pharyngeal tubercle [ PT ] , blue
rings = lateral pharyngeal tubercle [
LPT]](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-7-320.jpg)
![Line along the lateral pharyngeal tubercle [ LPT ] passes through Jugular
tubercle [ JT ] – so when you are drilling LPT in anterior skull base you will
land up on JT .
yellow ring = pharyngeal tubercle [ PT ] , blue rings = lateral pharyngeal
tubercle [ LPT] , green ring = Jugular tubercle](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-8-320.jpg)
![Lower clivus devided into
1. tubercular compartment [ Above red line ]
2. condylar compartment [ Below red line ]
Hypoglossal canal present at the junction of anterior 1/3rd & posterior 2/3rd](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-10-320.jpg)
![Lower clivus + petrous bone [ base ]
Petrous
bone
devided
into three
1/3rds](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-11-320.jpg)
![Lower clivus + petrous bone [ base ] + Zygomatic bone
Petrous bone devided
into three 1/3rds](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-12-320.jpg)

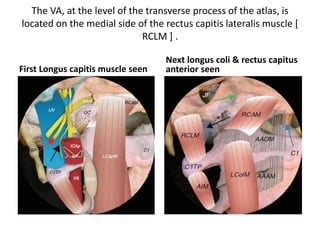
![The VA, at the level of the transverse process of the atlas, is
located on the medial side of the rectus capitis lateralis muscle [
RCLM ] .
First Longus capitis muscle seen
Next longus coli & rectus capitus
anterior seen](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-16-320.jpg)
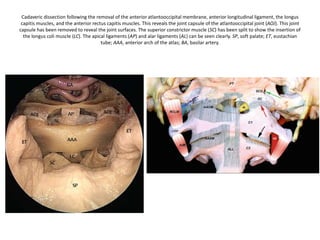
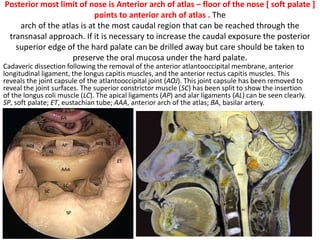
![Posterior most limit of nose is Anterior arch of atlas – floor of the nose [ soft palate ]
points to anterior arch of atlas . The
arch of the atlas is at the most caudal region that can be reached through the
transnasal approach. If it is necessary to increase the caudal exposure the posterior
superior edge of the hard palate can be drilled away but care should be taken to
preserve the oral mucosa under the hard palate.
Cadaveric dissection following the removal of the anterior atlantooccipital membrane, anterior
longitudinal ligament, the longus capitis muscles, and the anterior rectus capitis muscles. This
reveals the joint capsule of the atlantooccipital joint (AOJ). This joint capsule has been removed to
reveal the joint surfaces. The superior constrictor muscle (SC) has been split to show the insertion
of the longus coli muscle (LC). The apical ligaments (AP) and alar ligaments (AL) can be seen clearly.
SP, soft palate; ET, eustachian tube; AAA, anterior arch of the atlas; BA, basilar artery.](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-33-320.jpg)
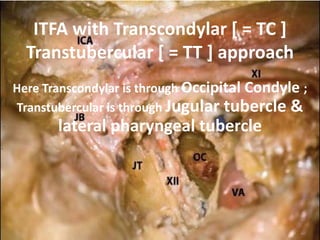
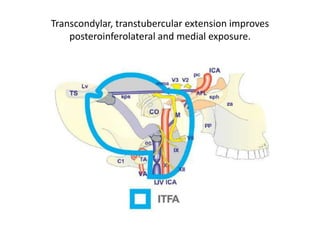
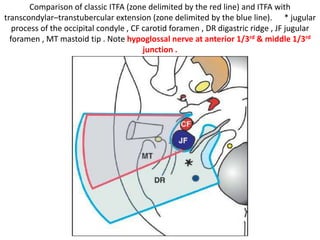

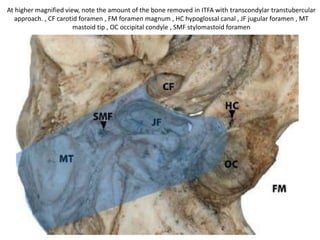

![ITFA with Transcondylar [ = TC ]
Transtubercular [ = TT ] approach
Here Transcondylar is through Occipital Condyle ;
Transtubercular is through Jugular tubercle &
lateral pharyngeal tubercle](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-52-320.jpg)
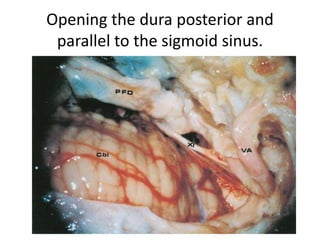
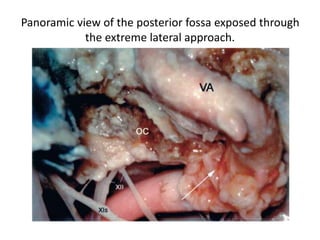
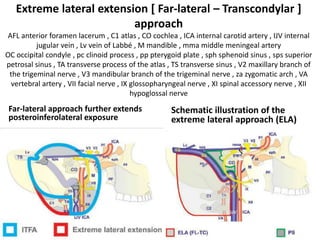
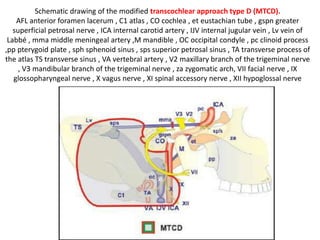
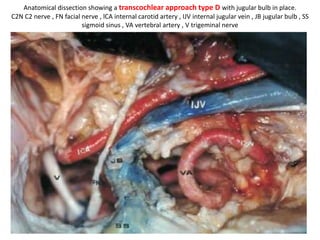
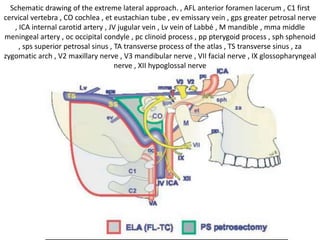
![Extreme lateral extension [ Far-lateral – Transcondylar ]
approach
AFL anterior foramen lacerum , C1 atlas , CO cochlea , ICA internal carotid artery , IJV internal
jugular vein , Lv vein of Labbé , M mandible , mma middle meningeal artery
OC occipital condyle , pc clinoid process , pp pterygoid plate , sph sphenoid sinus , sps superior
petrosal sinus , TA transverse process of the atlas , TS transverse sinus , V2 maxillary branch of
the trigeminal nerve , V3 mandibular branch of the trigeminal nerve , za zygomatic arch , VA
vertebral artery , VII facial nerve , IX glossopharyngeal nerve , XI spinal accessory nerve , XII
hypoglossal nerve
Far-lateral approach further extends
posteroinferolateral exposure
Schematic illustration of the
extreme lateral approach (ELA)](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-55-320.jpg)
![Lower clivus + petrous bone [ base ]
Petrous
bone
devided
into three
1/3rds](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-60-320.jpg)
![Lower clivus + petrous bone [ base ] + Zygomatic bone
Petrous bone devided
into three 1/3rds](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-61-320.jpg)

![The VA, at the level of the transverse process of the atlas, is
located on the medial side of the rectus capitis lateralis muscle [
RCLM ] .
First Longus capitis muscle seen
Next longus coli & rectus capitus
anterior seen](https://image.slidesharecdn.com/cranio-vertebraljunction360-150315230628-conversion-gate01/85/Cranio-vertebral-junction-Foramen-magnum-360-90-320.jpg)