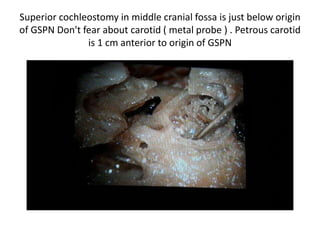
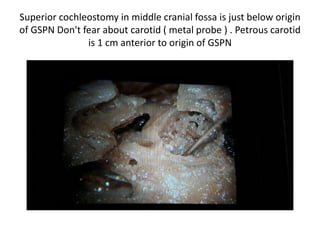
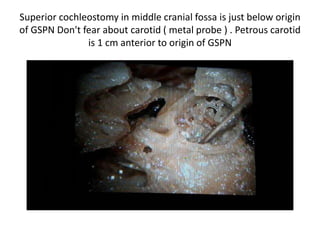
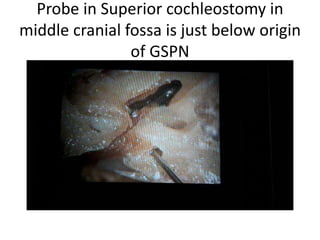
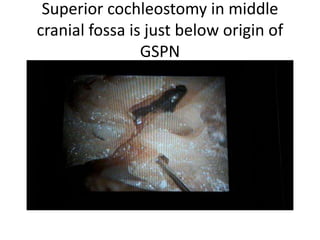
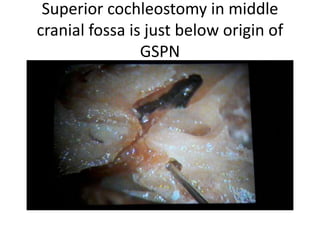
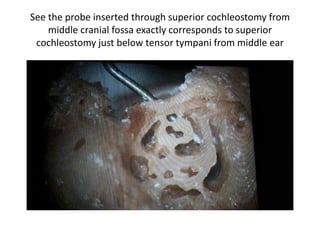
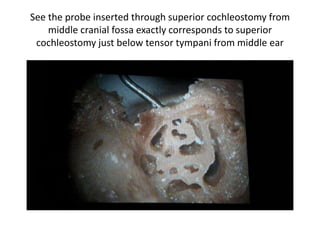
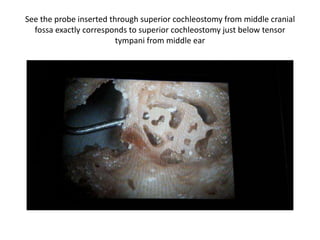
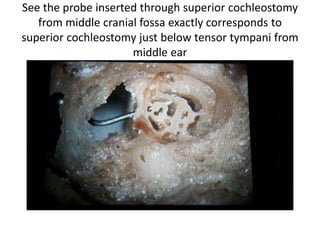
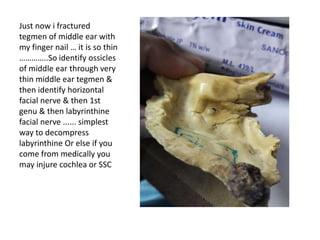
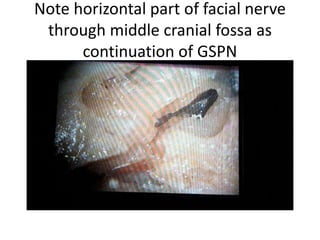
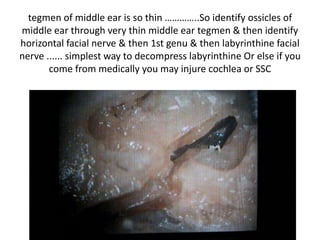
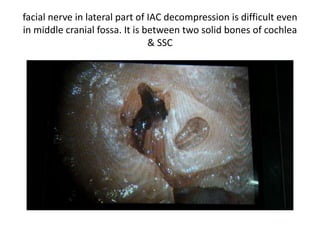
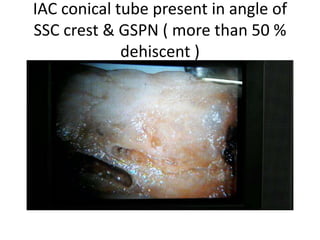
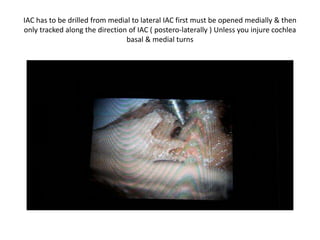
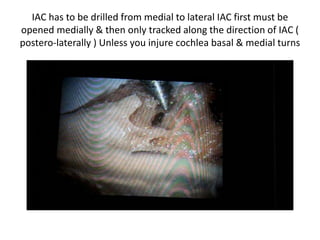
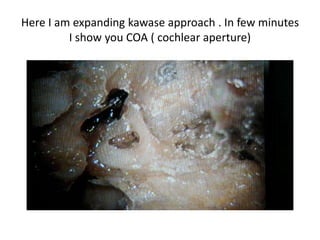
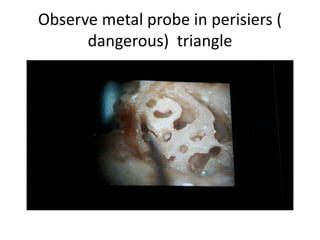
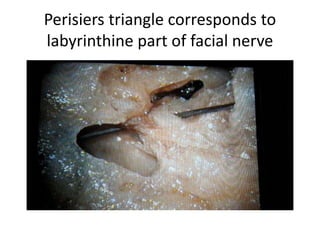
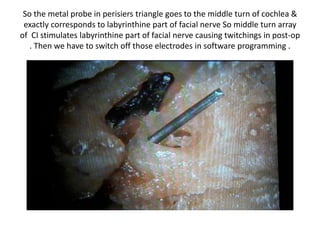
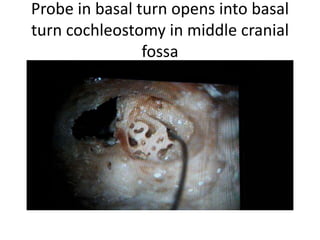
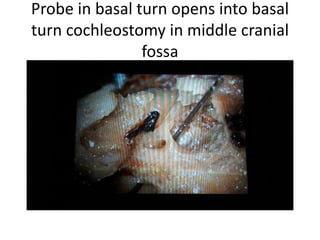
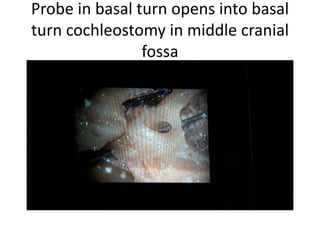
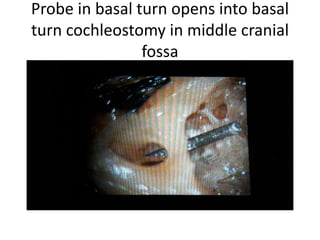
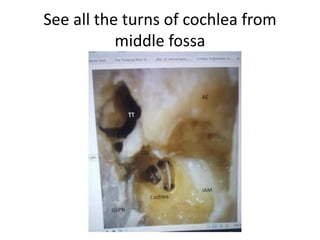
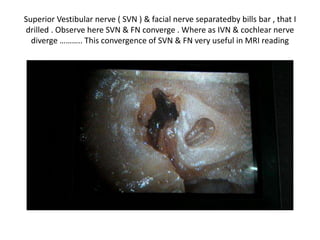
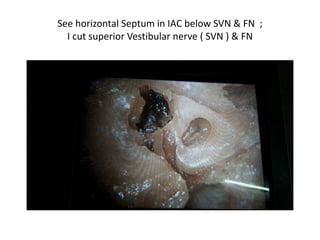
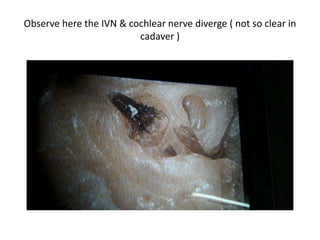
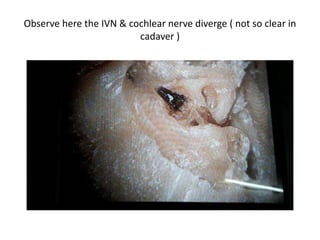
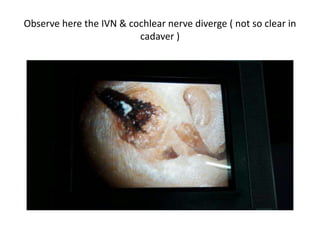
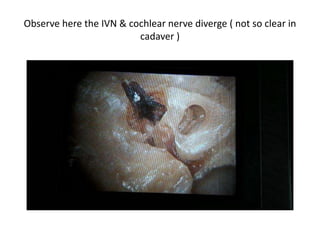
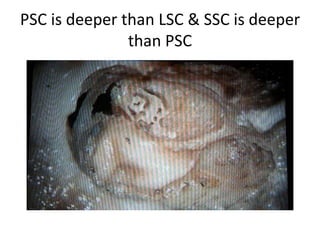
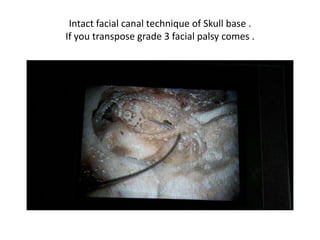
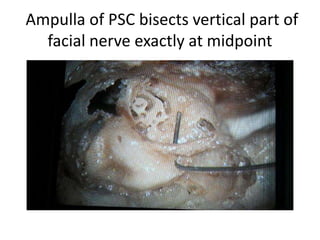
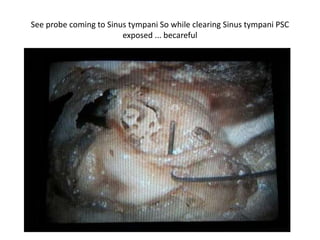
This document discusses techniques for cochlear implantation through the middle cranial fossa approach. It describes performing a superior cochleostomy just below the origin of the greater superficial petrosal nerve. It cautions not to fear injury to the carotid artery, which is 1 cm anterior. It also details identifying structures like the facial nerve and drilling the internal auditory canal from medial to lateral to avoid injuring the cochlea. Electrodes are described being placed in the basal, middle, and apical turns of the cochlea. Facial nerve stimulation is a risk if electrodes contact the labyrinthine segment, so selective deactivation may be needed. The document emphasizes the importance of anatomical landmarks and







![IAC [ Internal Auditory Canal ]
Drilling](https://image.slidesharecdn.com/cochleacadaverdissection-part2-170418142225/85/Cochlea-cadaver-dissection-part-2-26-320.jpg)








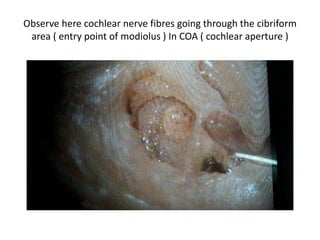
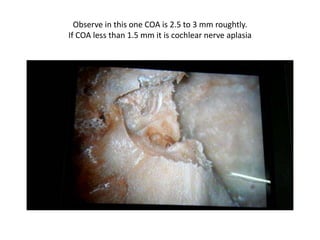
![COA [ Cochlear aperture ]](https://image.slidesharecdn.com/cochleacadaverdissection-part2-170418142225/85/Cochlea-cadaver-dissection-part-2-68-320.jpg)













![VA [ Vestibular Aqueduct ]](https://image.slidesharecdn.com/cochleacadaverdissection-part2-170418142225/85/Cochlea-cadaver-dissection-part-2-92-320.jpg)

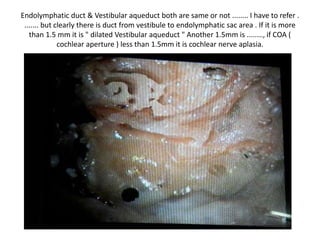
![anatomically also after drilling PSC we are seeing VA .... so radiologically also
both sizes same [ my mnemonic & philosophy ] ..... if VA more than PSC it is
dilated](https://image.slidesharecdn.com/cochleacadaverdissection-part2-170418142225/85/Cochlea-cadaver-dissection-part-2-101-320.jpg)