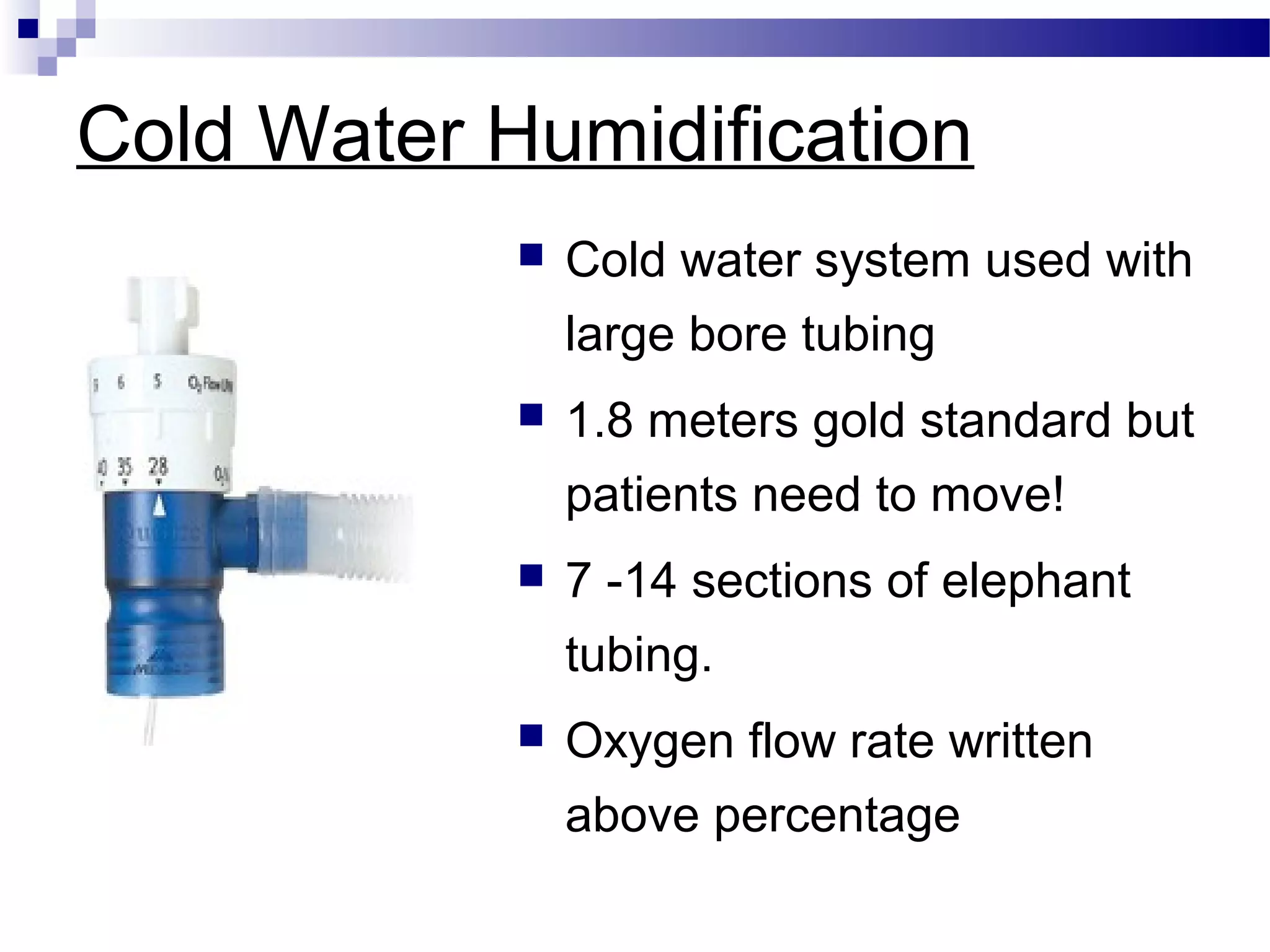
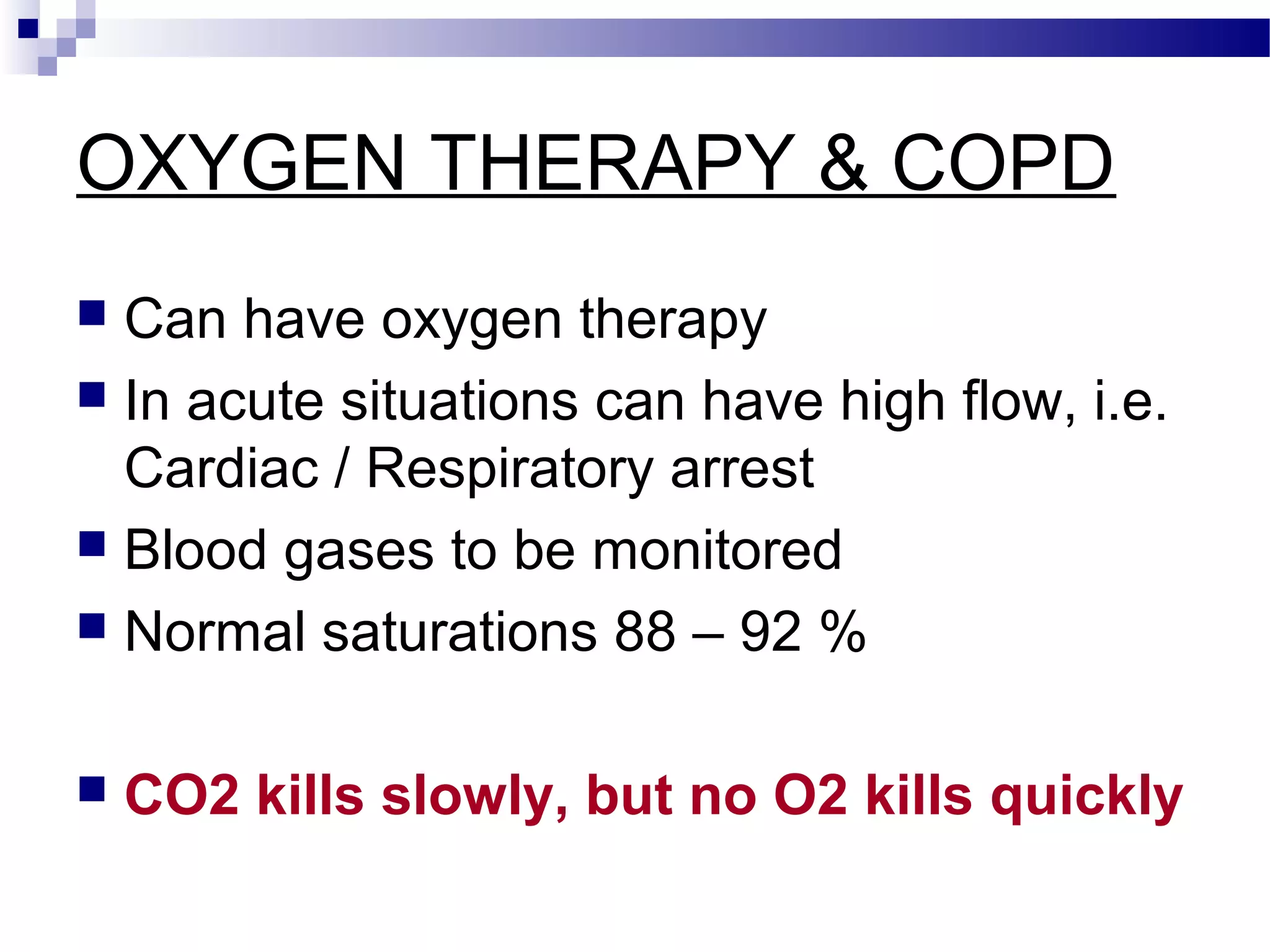
The document provides information about a core skills study day on physiological observations and oxygen therapy led by Mr. Shibu Chacko from the Critical Care Outreach Team. It discusses monitoring temperature, pulse, blood pressure, respiration rate, oxygen saturation and various scores. It also covers different oxygen delivery systems including nasal cannula, face masks, non-rebreathing masks and venturi masks. The importance of humidification with prolonged oxygen therapy is highlighted along with monitoring patients on oxygen therapy.