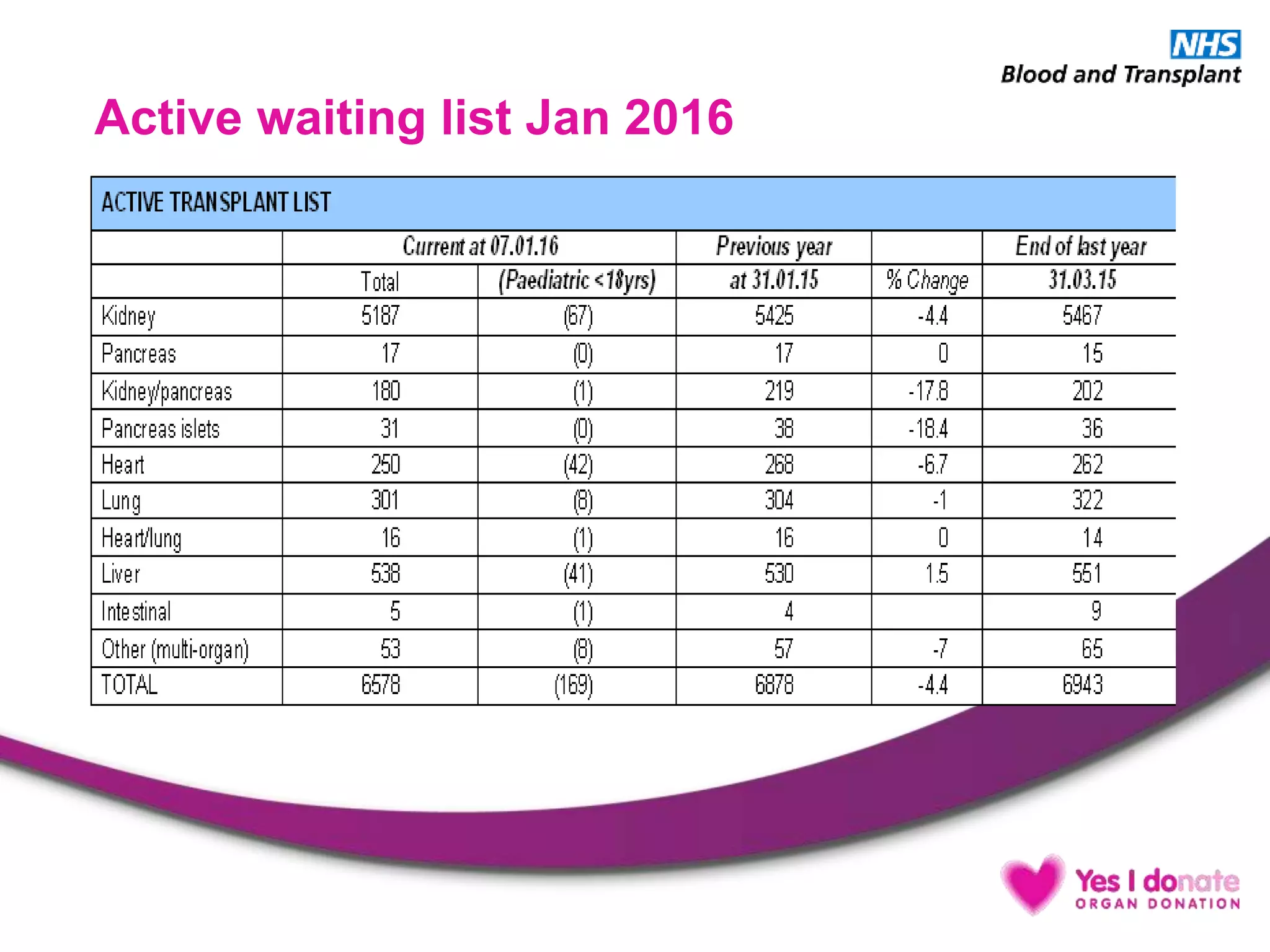
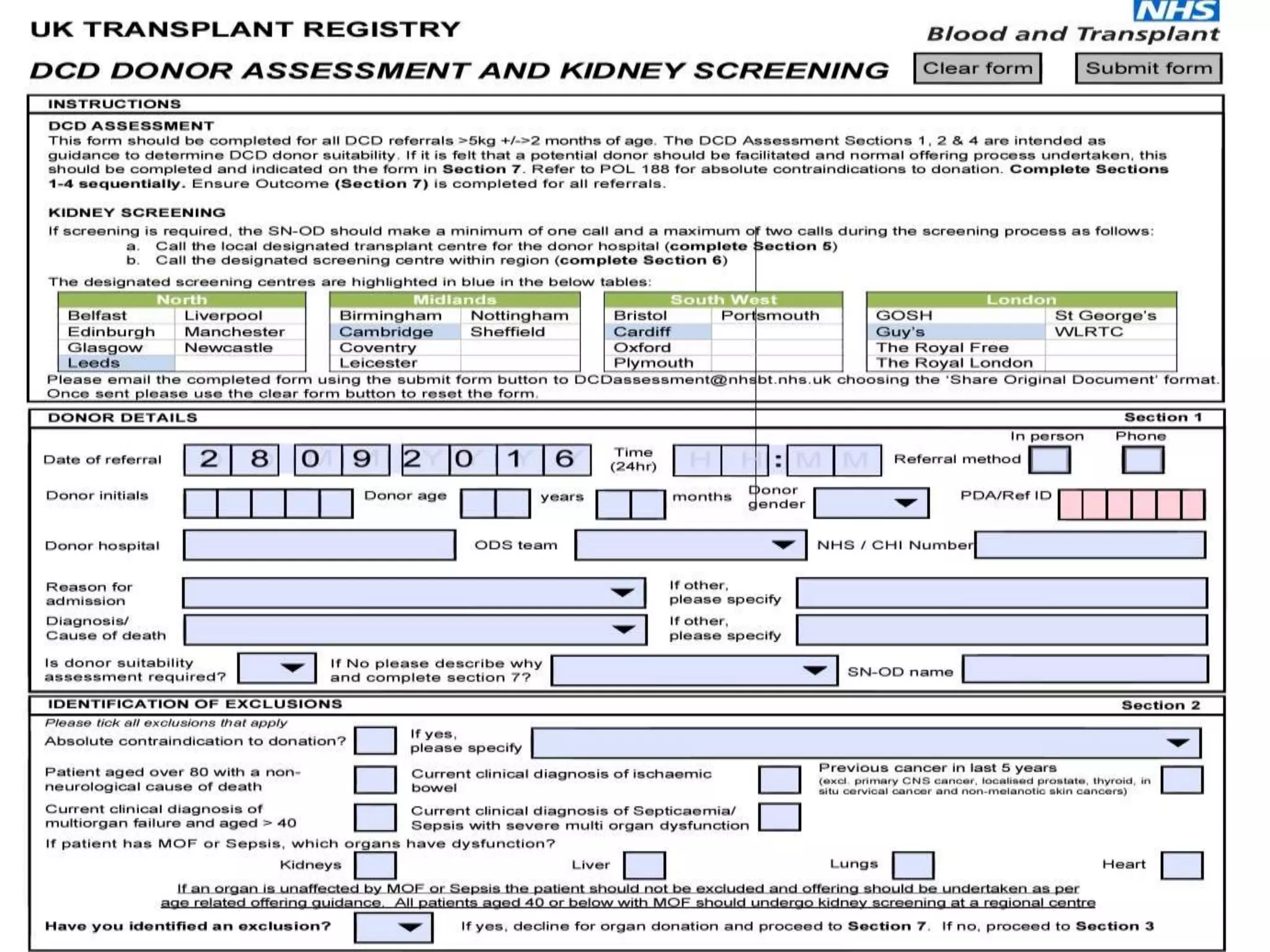
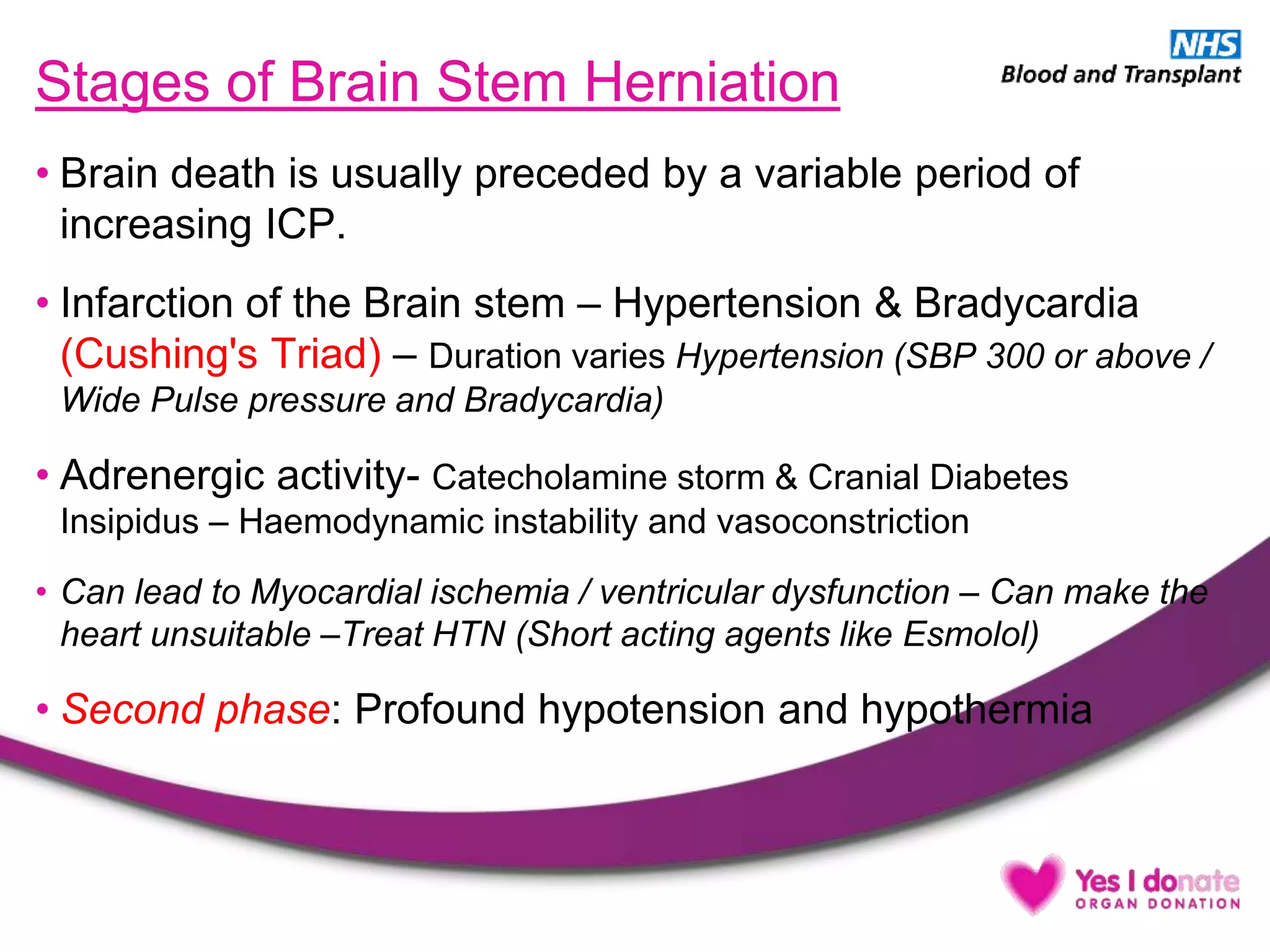
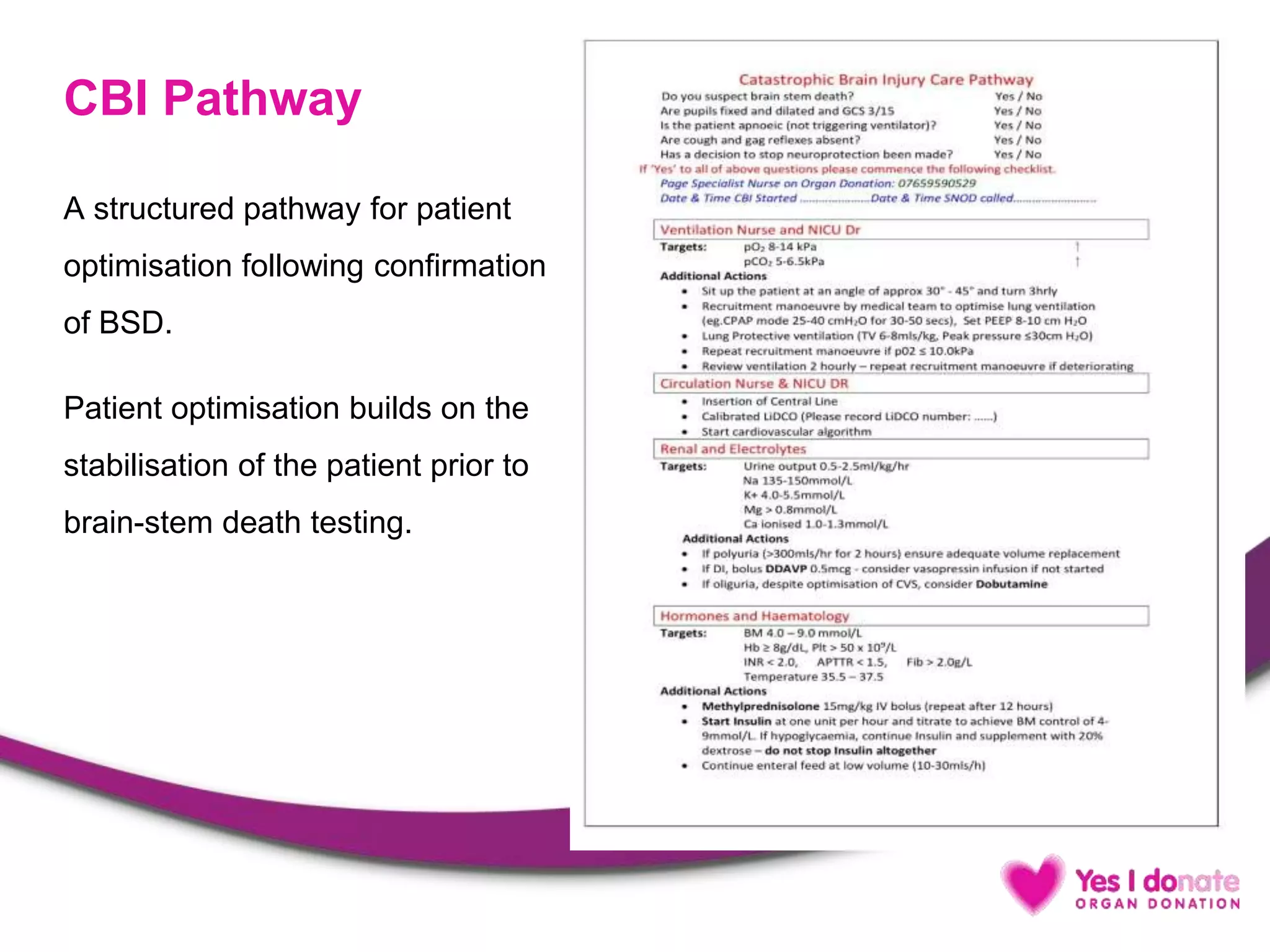
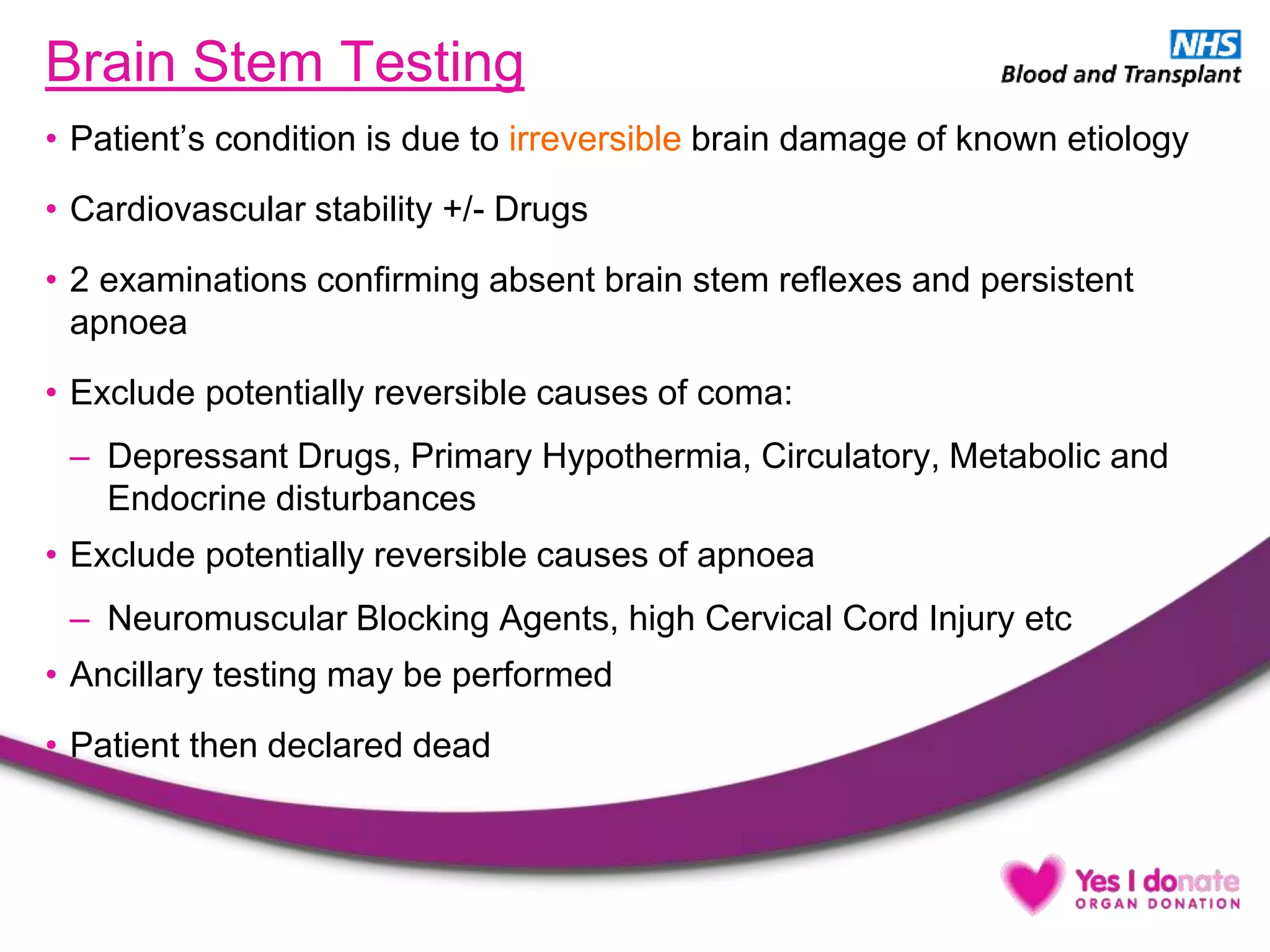
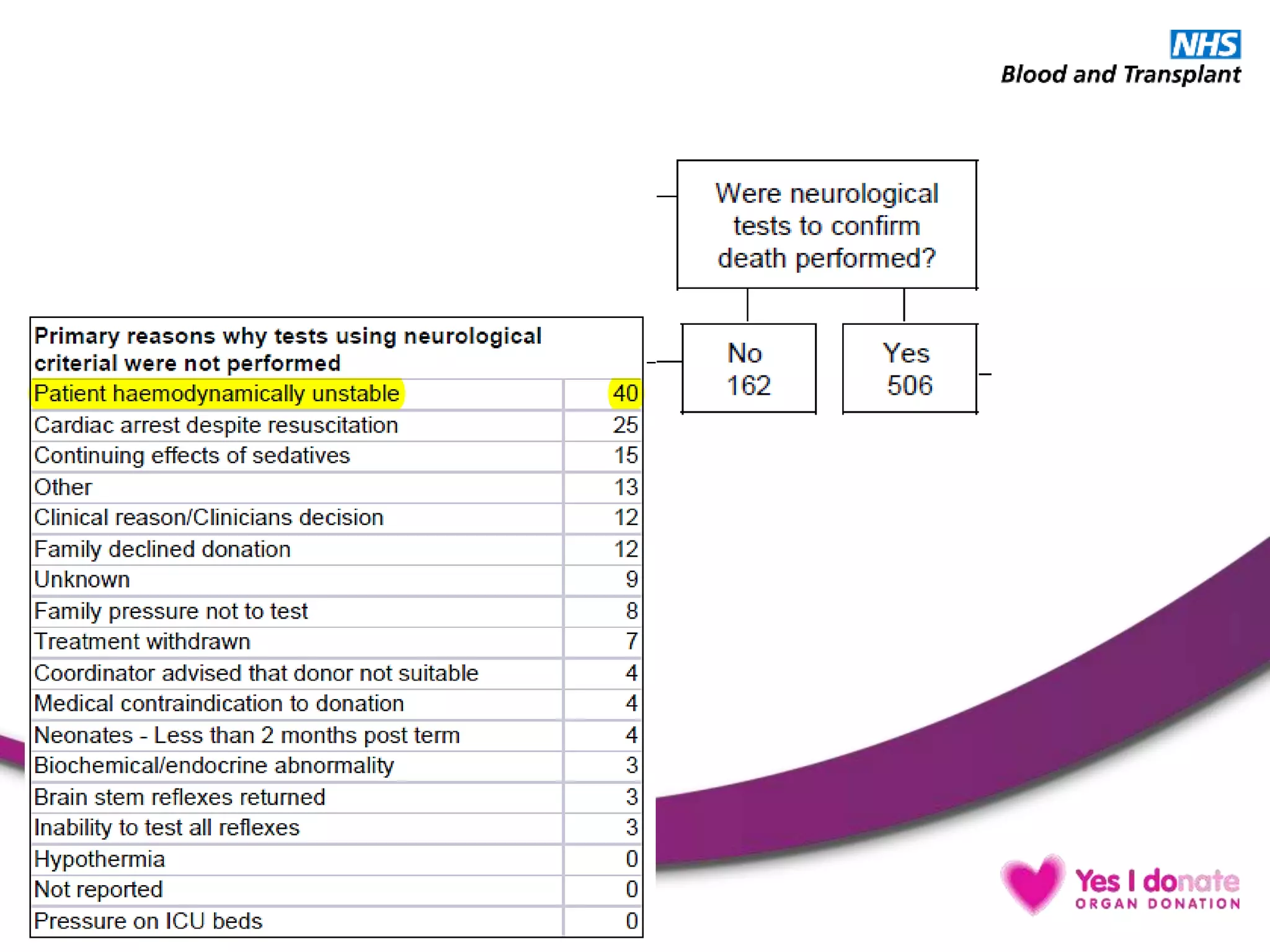
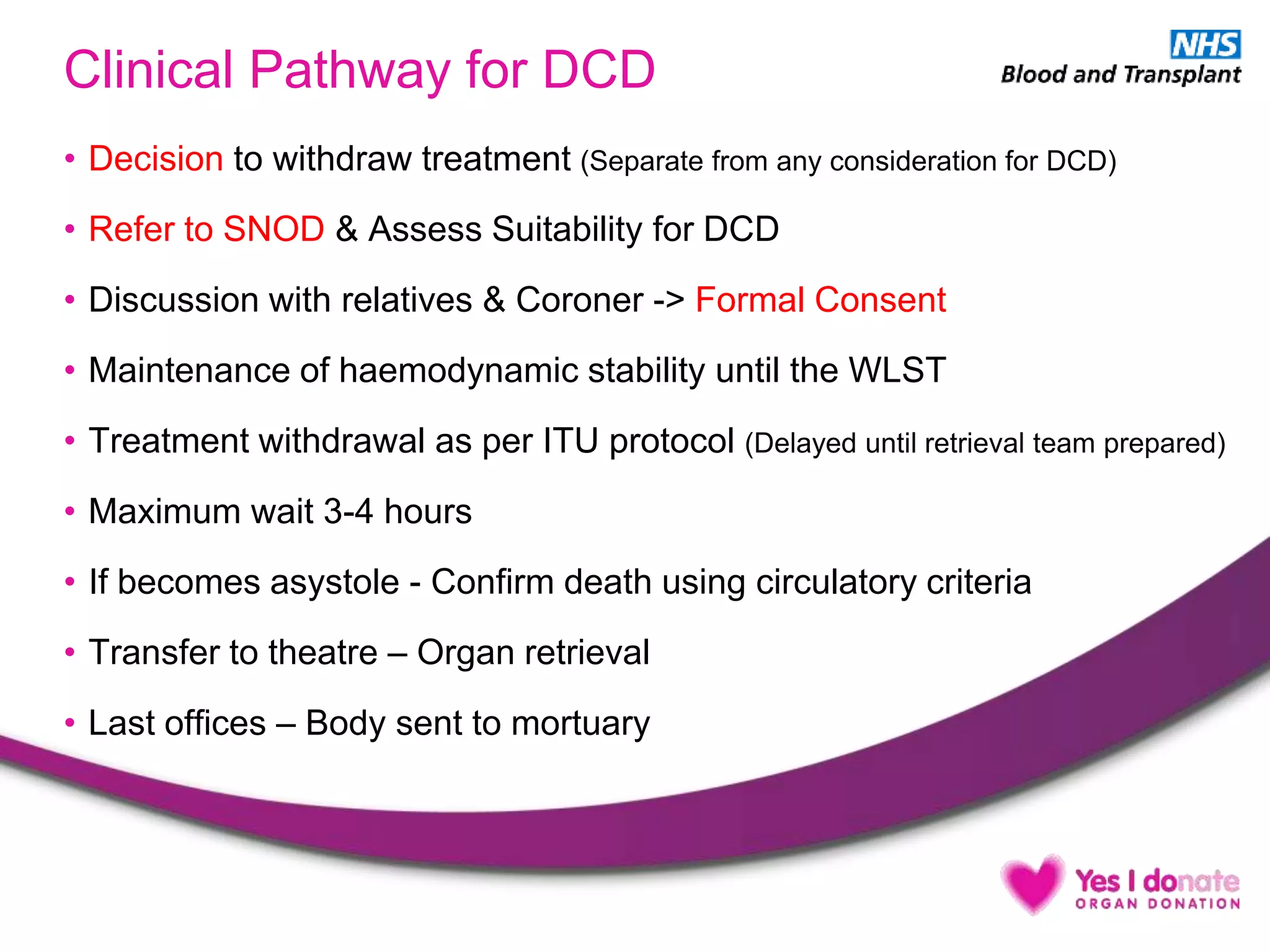
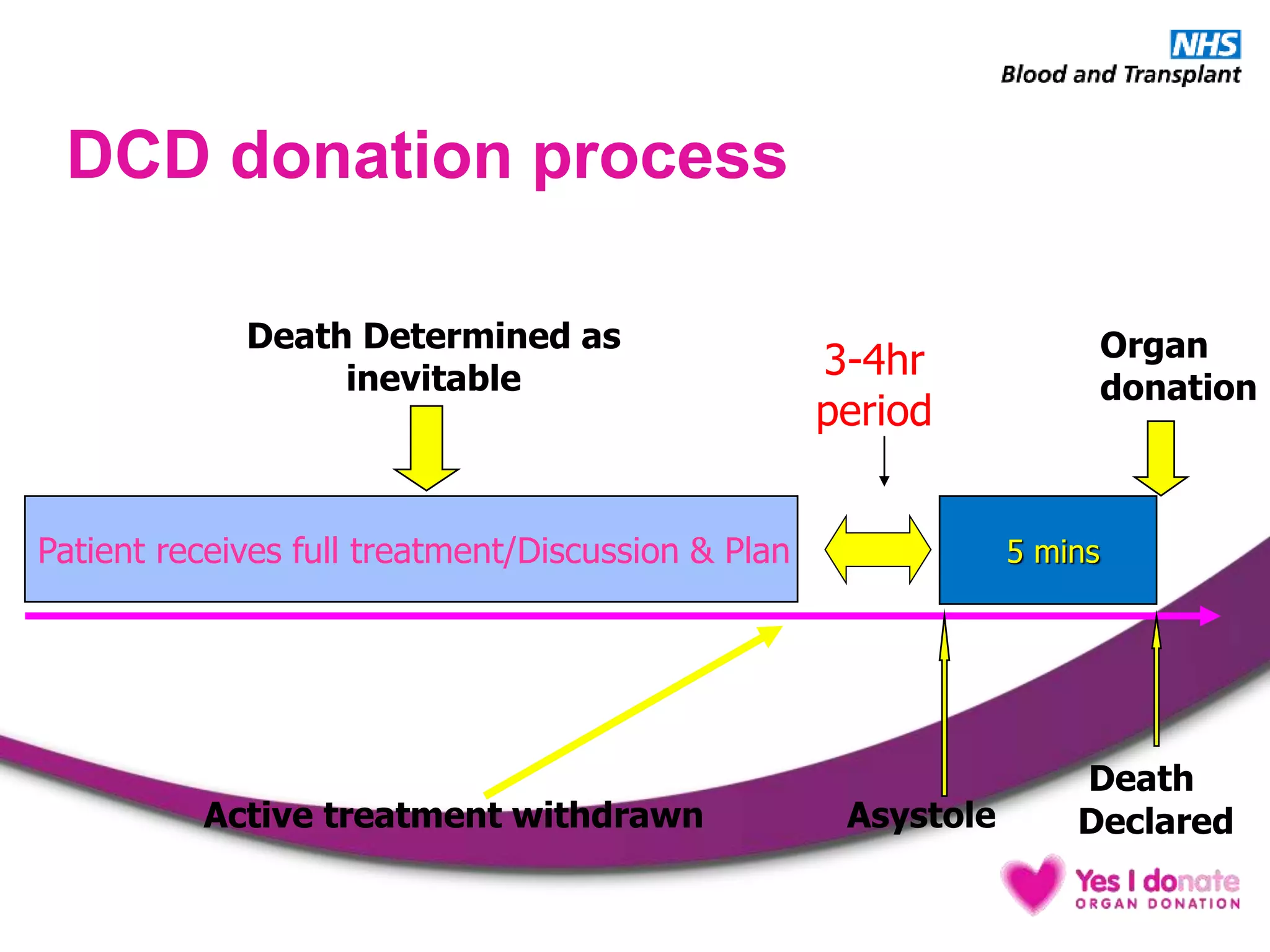
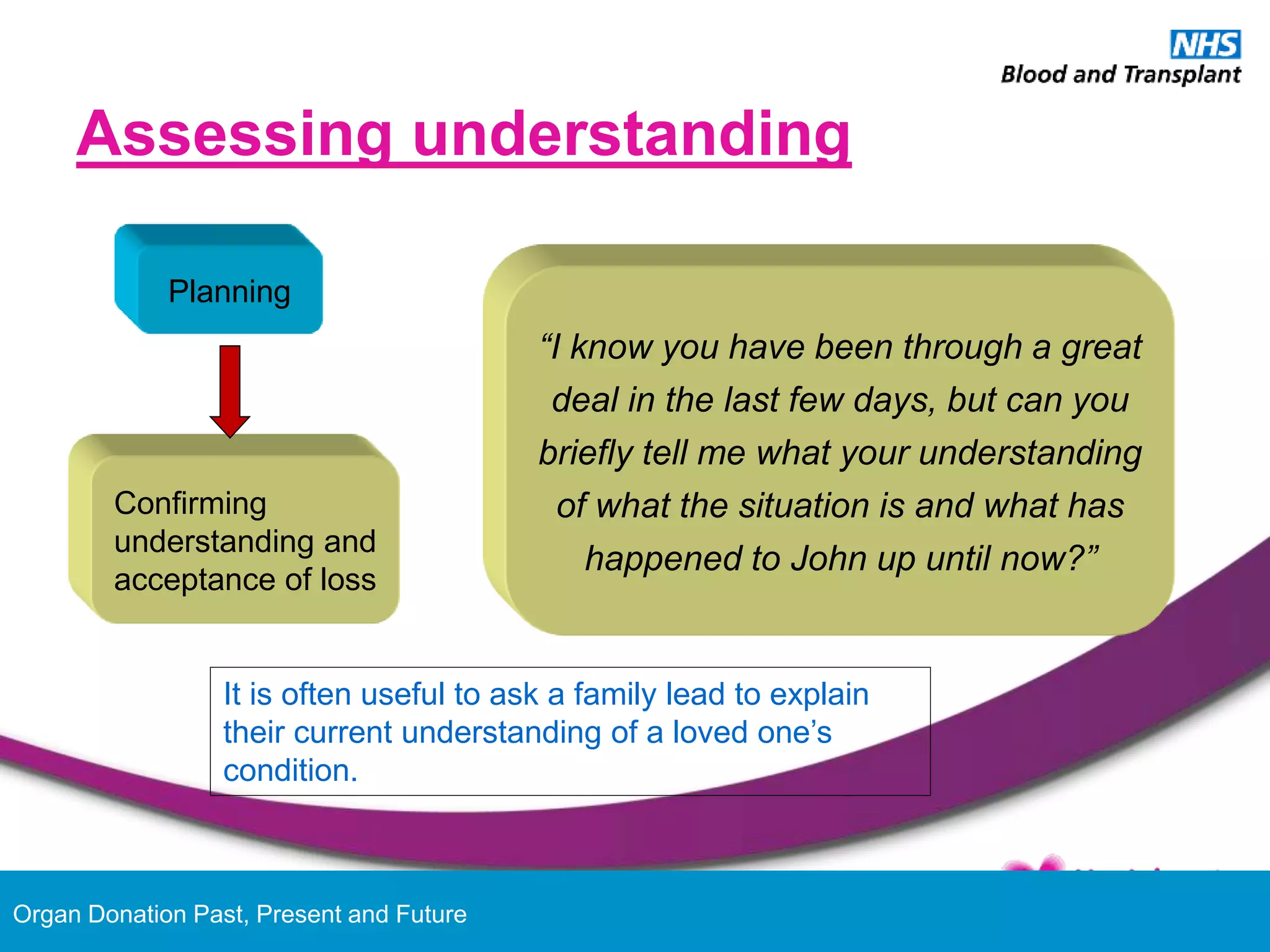
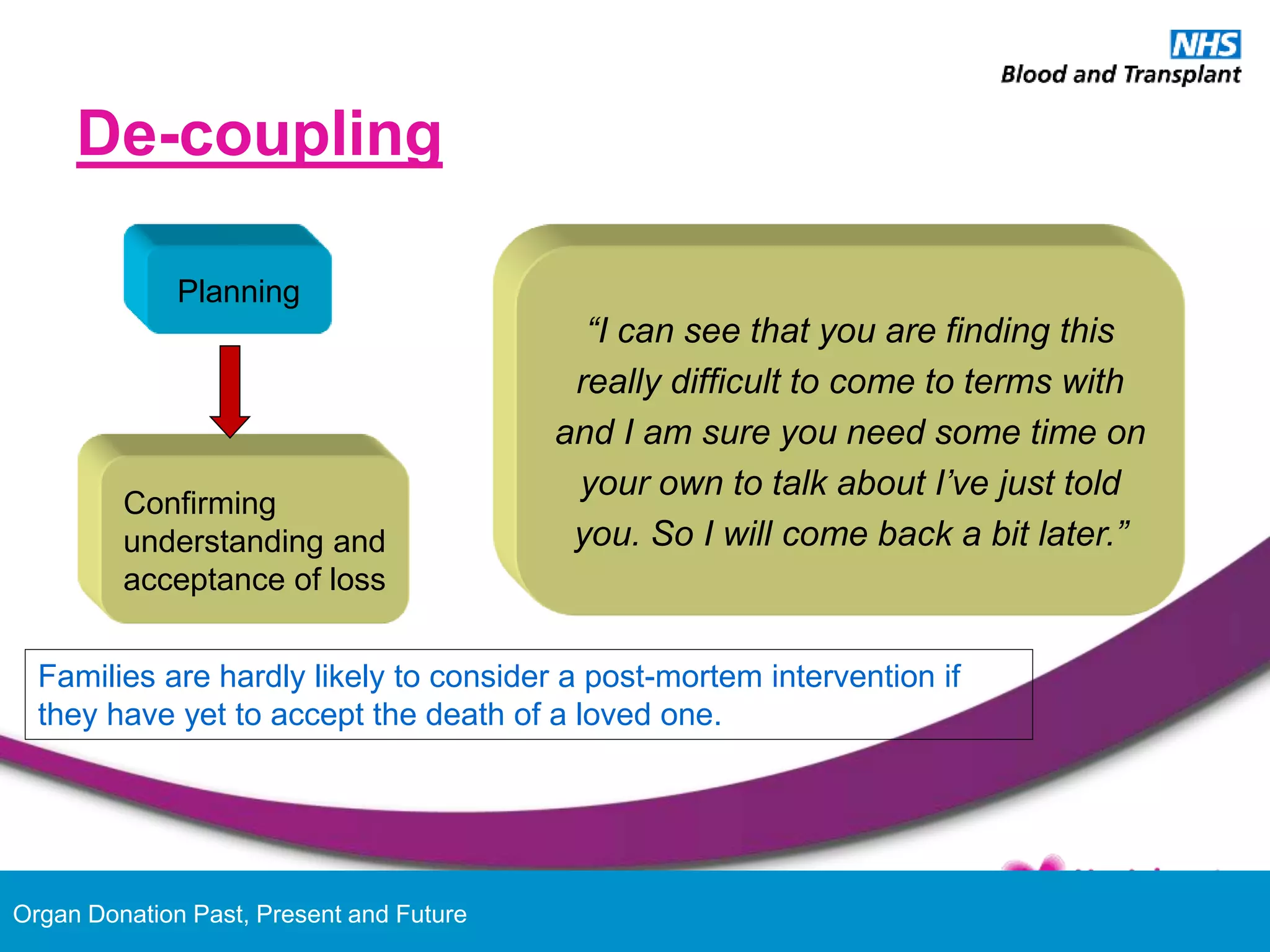
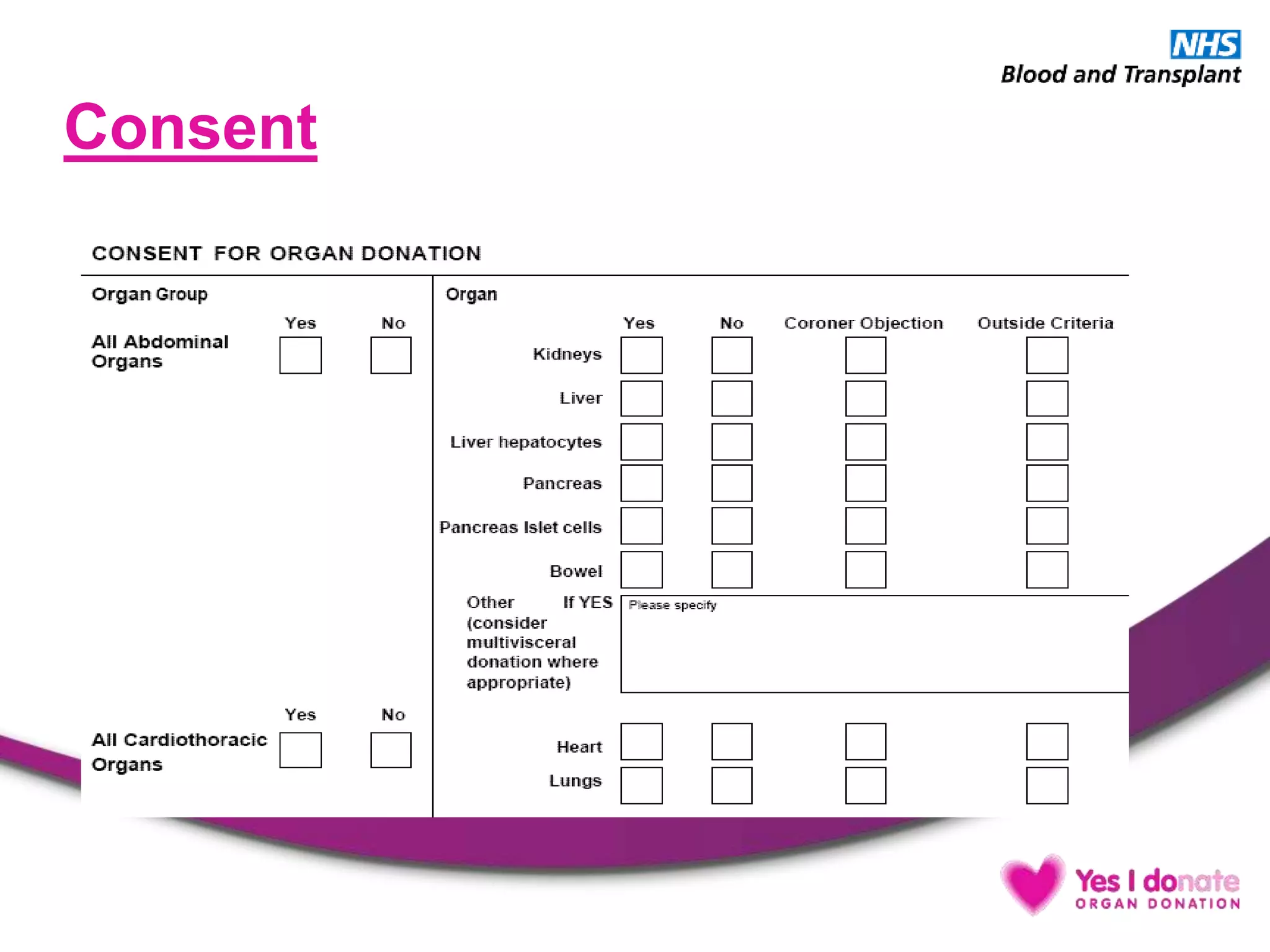
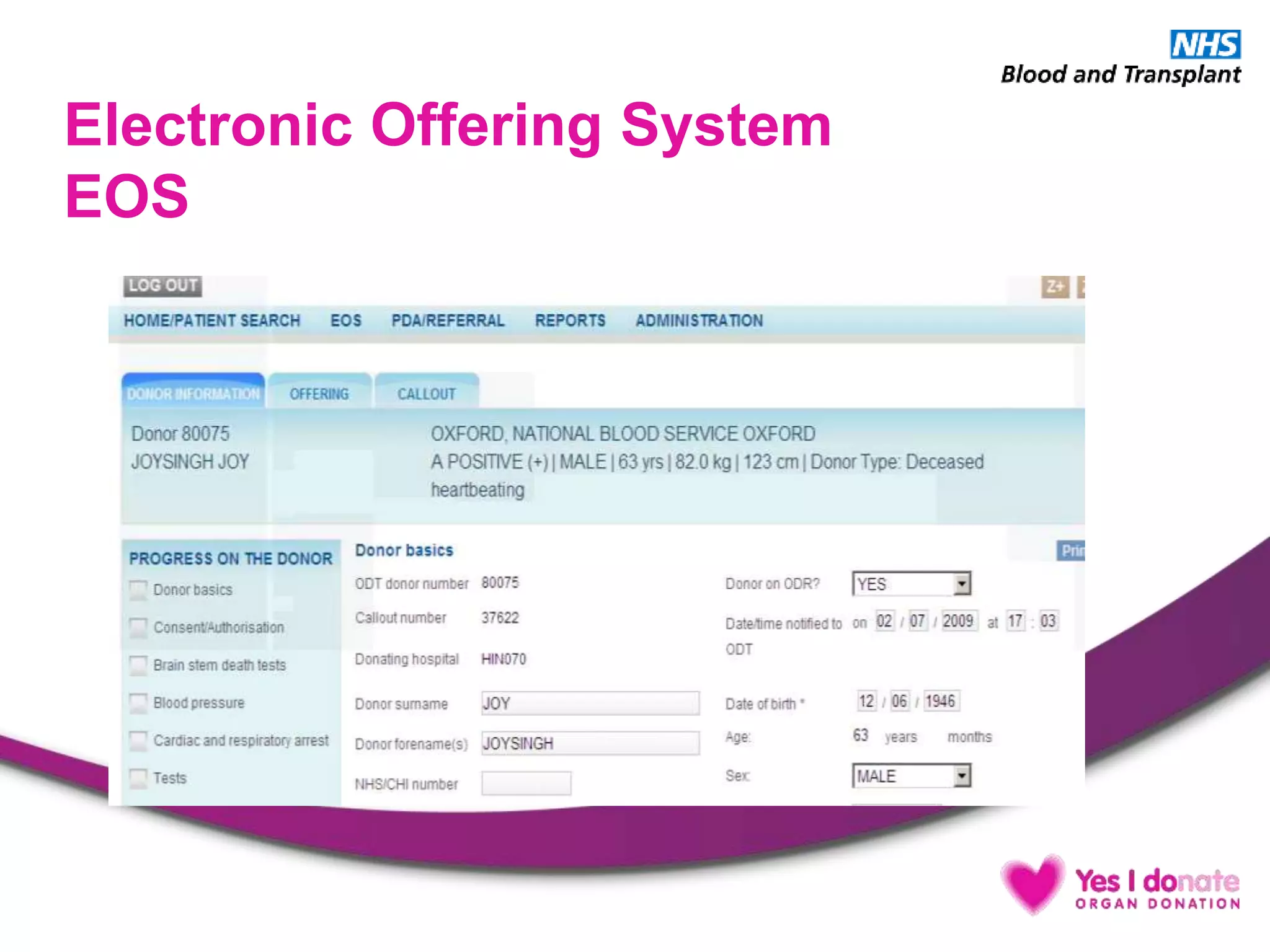
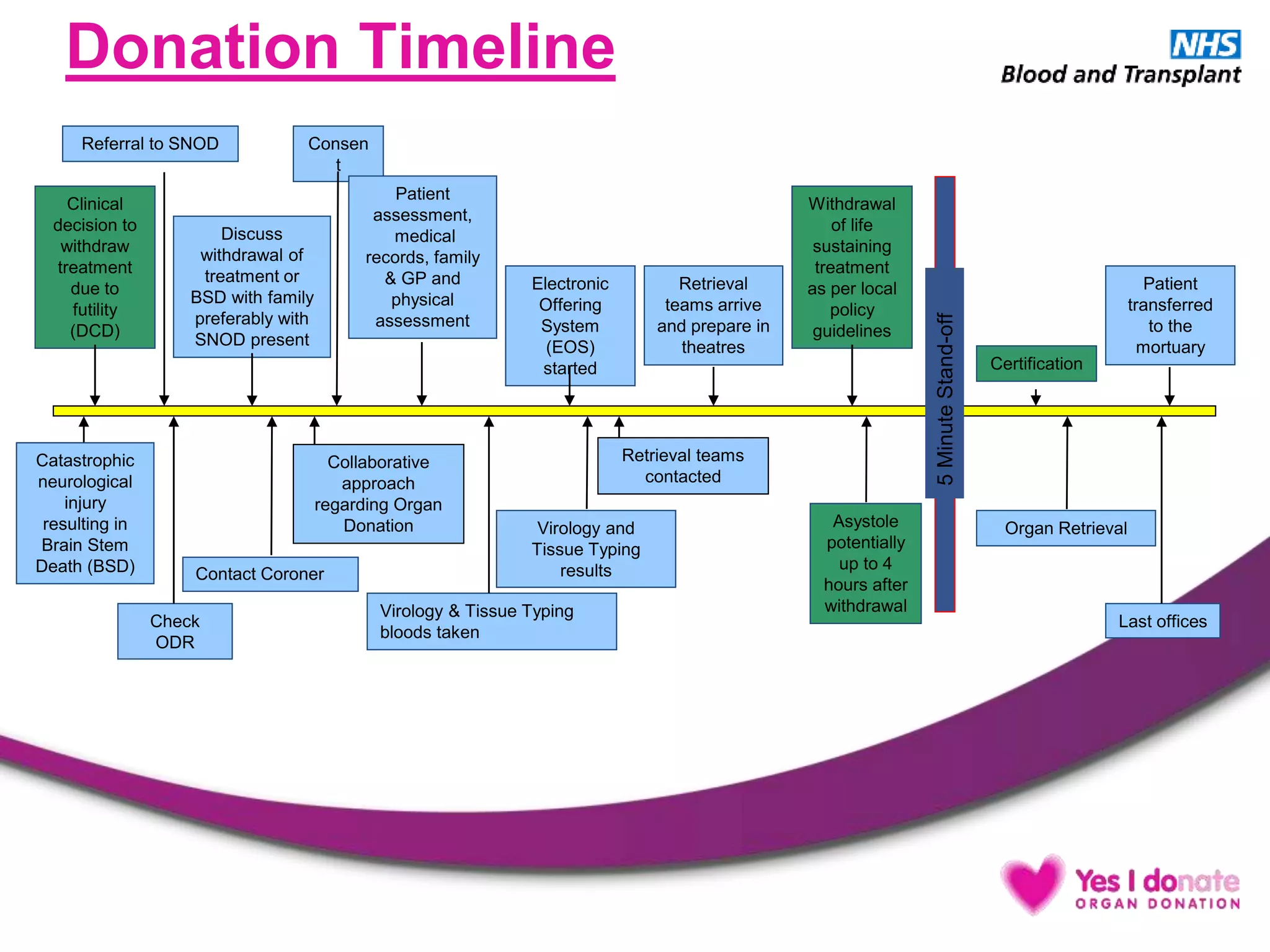
This document provides information on organ and tissue donation. It begins with definitions and an overview of organ donation terminology. Statistics are presented showing the potential for donation in the UK and barriers that currently exist. The document then describes the different types of donation including living donation, donation after brainstem death, and donation after circulatory death. Key aspects of the donation process are explained including donor identification, screening, management, and the brainstem death testing procedure. Overall the document aims to educate about organ donation by defining terms, presenting statistics, and explaining the clinical process.