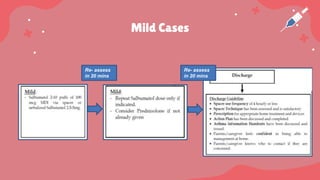
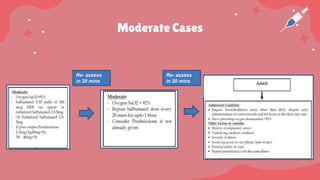
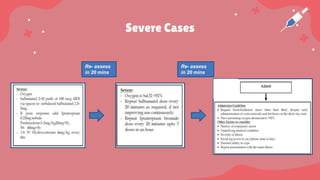
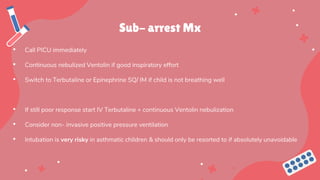
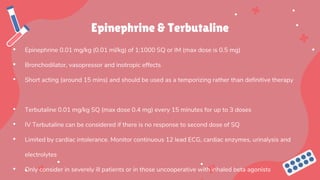
Maryam, a 5-year-old girl with a recent asthma diagnosis, presented to the emergency department with worsening respiratory distress following three days of upper respiratory symptoms. Examination revealed signs of moderate asthma exacerbation, including wheezing and agitation, as well as vital signs indicating tachypnea and hypoxia. Treatment began with supplemental oxygen and nebulizations, and in severe cases, further interventions such as IV corticosteroids and magnesium sulfate may be required.