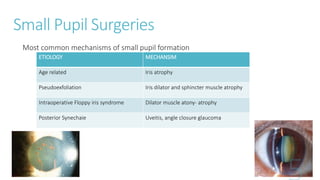
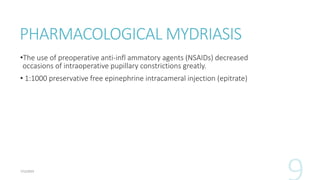
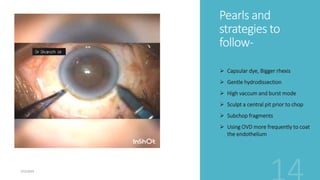
The document discusses complex cases in cataract surgery, focusing on small pupil surgeries, hard cataracts, posterior polar cataracts, and cataracts associated with Fuchs' corneal dystrophy. It emphasizes the importance of recognizing high-risk eyes and utilizing various pharmacological and mechanical management strategies to reduce complications. The document also outlines surgical techniques and advancements in equipment to improve outcomes for challenging cataract cases.
















![Cataract with Fuch’s endothelial
dystrophy
Fuchs’ endothelial corneal dystrophy (FECD) is a condition that affects the corneal endothelium,
resulting in a reduction in the number of Na+/K+ ATPase pumps [1]. Clinically, this manifests as corneal
edema, which can lead to symptomatic glare and halos, and ultimately decreased visual acuity.
Presentation- blurring of vision (more in the morning hours), glare.
Detection- guttae
External Disease and Cornea, Section 8. Basic Clinical Science Course, American Academy of Ophthalmology. 2018.](https://image.slidesharecdn.com/editedcomplexcasesincataractsurgeryanditsmanagement-230712063312-2f908797/85/Complex-cases-in-Cataract-surgery-and-its-management-pptx-20-320.jpg)