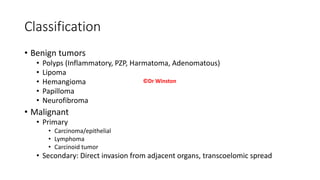
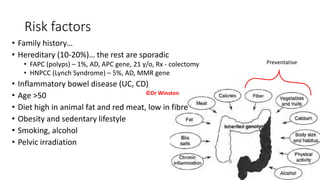
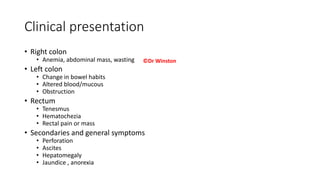
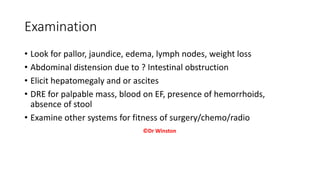
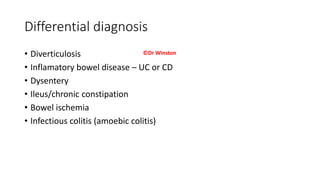
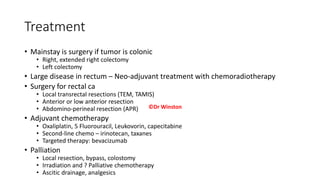
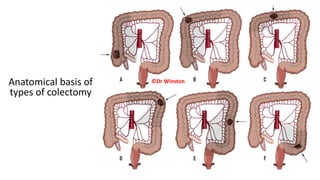
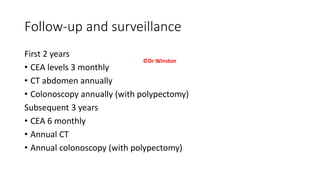
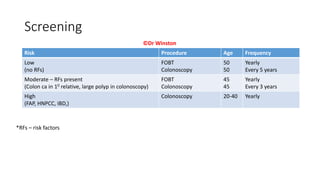
Colorectal cancer is the third most common cancer worldwide and in Kenya. It occurs due to uncontrolled cell growth in the colon. Risk factors include family history, inflammatory bowel disease, older age, diet high in red meat and low in fiber, obesity, smoking, and alcohol. Staging involves classifying the tumor size and spread, with stage 4 being tumors that have metastasized to distant organs. Treatment depends on location and stage of the cancer, and may involve surgery, chemotherapy, and radiation therapy. Follow-up care includes regular blood tests, imaging scans, and colonoscopies to monitor for recurrence or spread of the cancer.