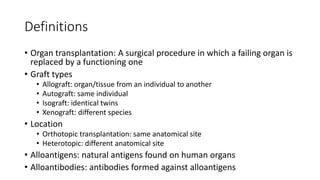
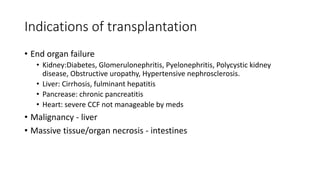
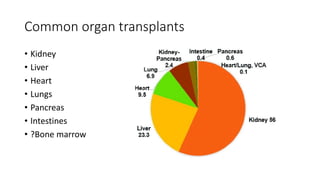
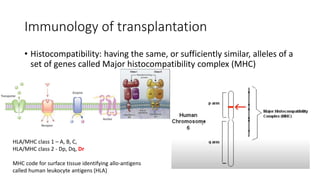
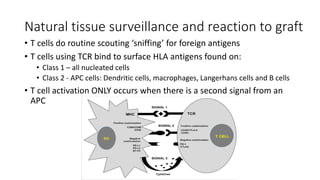
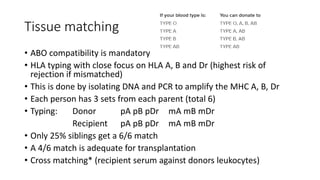
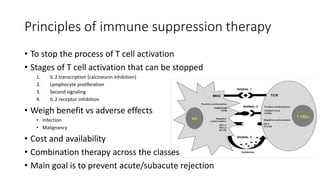
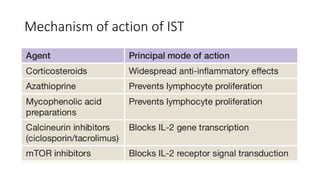
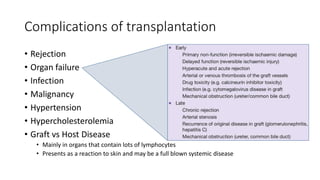
This document provides an overview of transplantation surgery principles. It defines key terms like transplantation, graft types, and alloantigens. It discusses indications for common organ transplants like kidney, liver, heart and lungs. It also covers the immunological basis for graft rejection, focusing on the role of the major histocompatibility complex and human leukocyte antigens in triggering rejection. Finally, it summarizes strategies for tissue matching between donors and recipients, principles of immunosuppressive therapy to prevent rejection, potential complications of transplantation, and methods for organ donation and preservation.