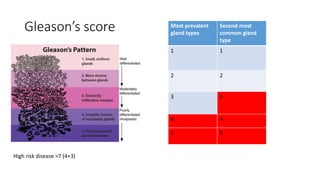
Prostate cancer is the most common cancer in men. It arises from the prostate gland and is dependent on androgens like testosterone for growth. Risk factors include increased age, family history, and race. Screening involves a digital rectal exam and PSA blood test. Biopsy confirms diagnosis. Staging uses the TNM system and Gleason score. Treatment options include active surveillance for low risk disease, surgery, radiation, hormone therapy, chemotherapy, and palliation depending on age, risk level, and whether the cancer has spread. The goal is cure of localized disease or palliation of symptoms from advanced disease.