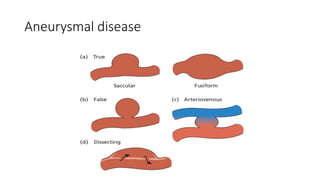
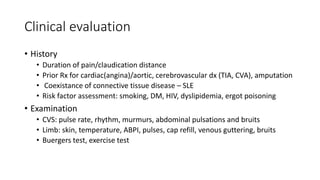
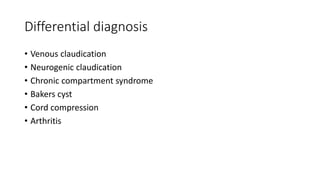
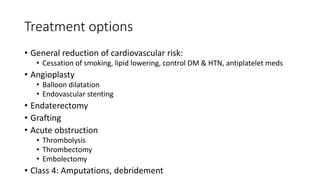
This document provides an overview of arterial vaso-occlusive disease. It discusses the surgical anatomy, physiology, epidemiology, etiology, work-up, treatment, and scope of diseases. Specific topics covered include arterial trauma, aneurysmal disease, the pathology and causes of vaso-occlusive disease, clinical presentation, classification systems, clinical evaluation, investigations, differential diagnosis, and treatment options such as angioplasty, stenting, grafting, thrombectomy, and amputation. The objectives are to review the anatomy, functions, screening, diagnosis, staging, and management of various arterial diseases involving occlusion.