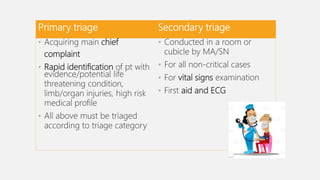
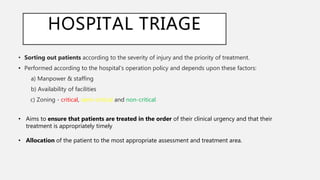
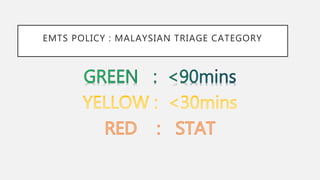
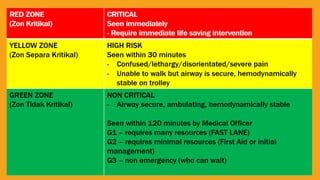
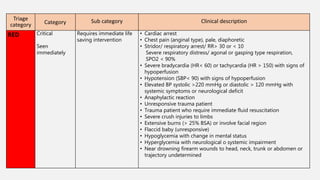
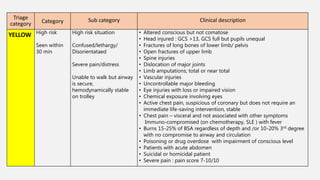
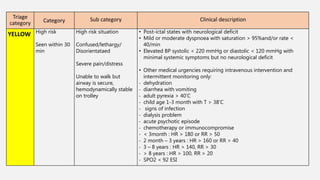
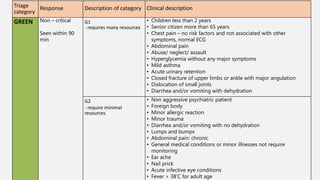
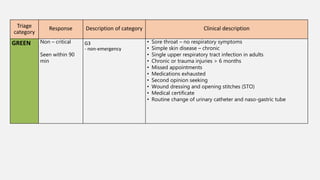
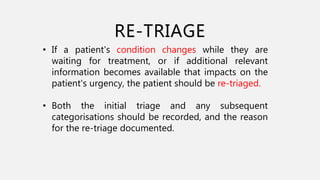
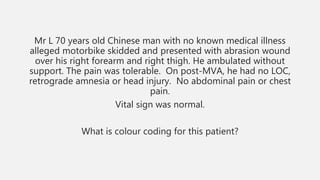
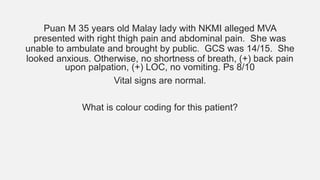
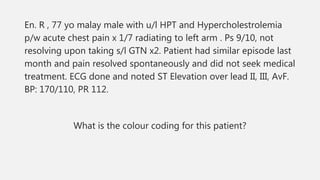
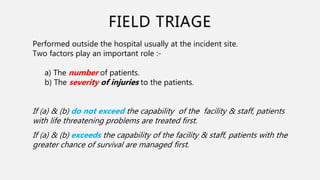
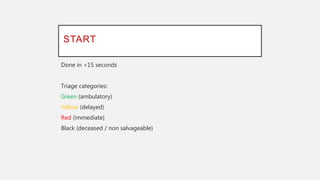
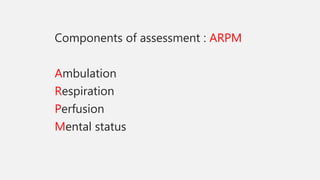
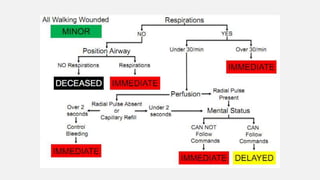
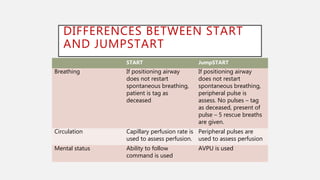
This document discusses different aspects of a triage system used in a hospital emergency department. It begins by defining triage and explaining the objectives of triage in an emergency setting. It then describes different levels of triage conducted, including primary and secondary triage, field triage, and hospital triage. Details are provided on how patients are categorized into different triage categories based on the urgency of their condition. The document also discusses triage tools used in field settings like START and JumpSTART triage. Overall, the document provides an overview of an emergency department's triage process and categorization of patients based on clinical need.