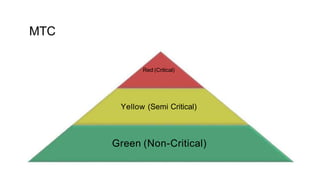
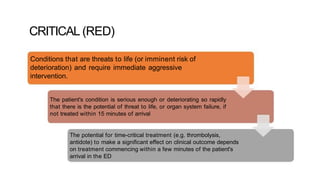
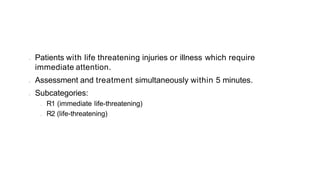
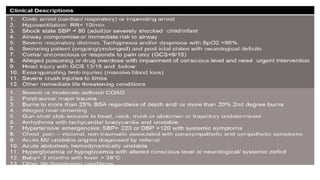
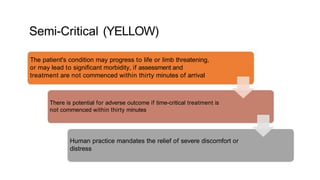
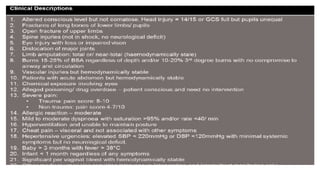
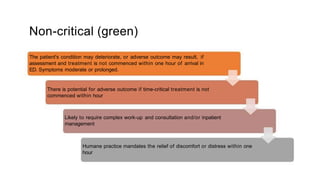
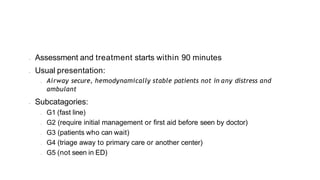
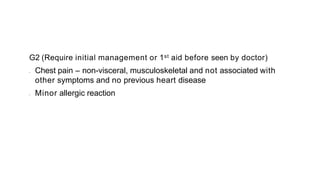
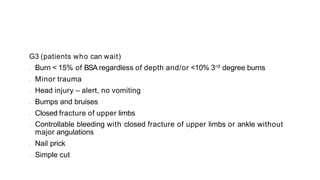
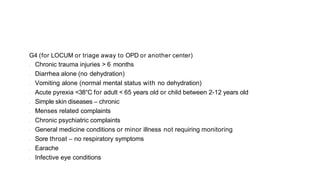
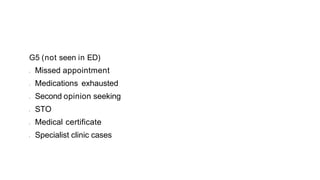
This document provides information on the Malaysian Triage Category (MTC) system used in emergency departments in Malaysia. The MTC system classifies patients into three categories - Red (Critical), Yellow (Semi-Critical), and Green (Non-Critical) - based on the urgency of their condition. The Red category includes life-threatening conditions requiring treatment within 5 minutes. Yellow indicates conditions that could become life-threatening without treatment within 30 minutes. Green covers non-emergent conditions treatable within 90 minutes. Each category has further subcategories to aid in prioritizing patient flow and resource allocation in emergency departments.