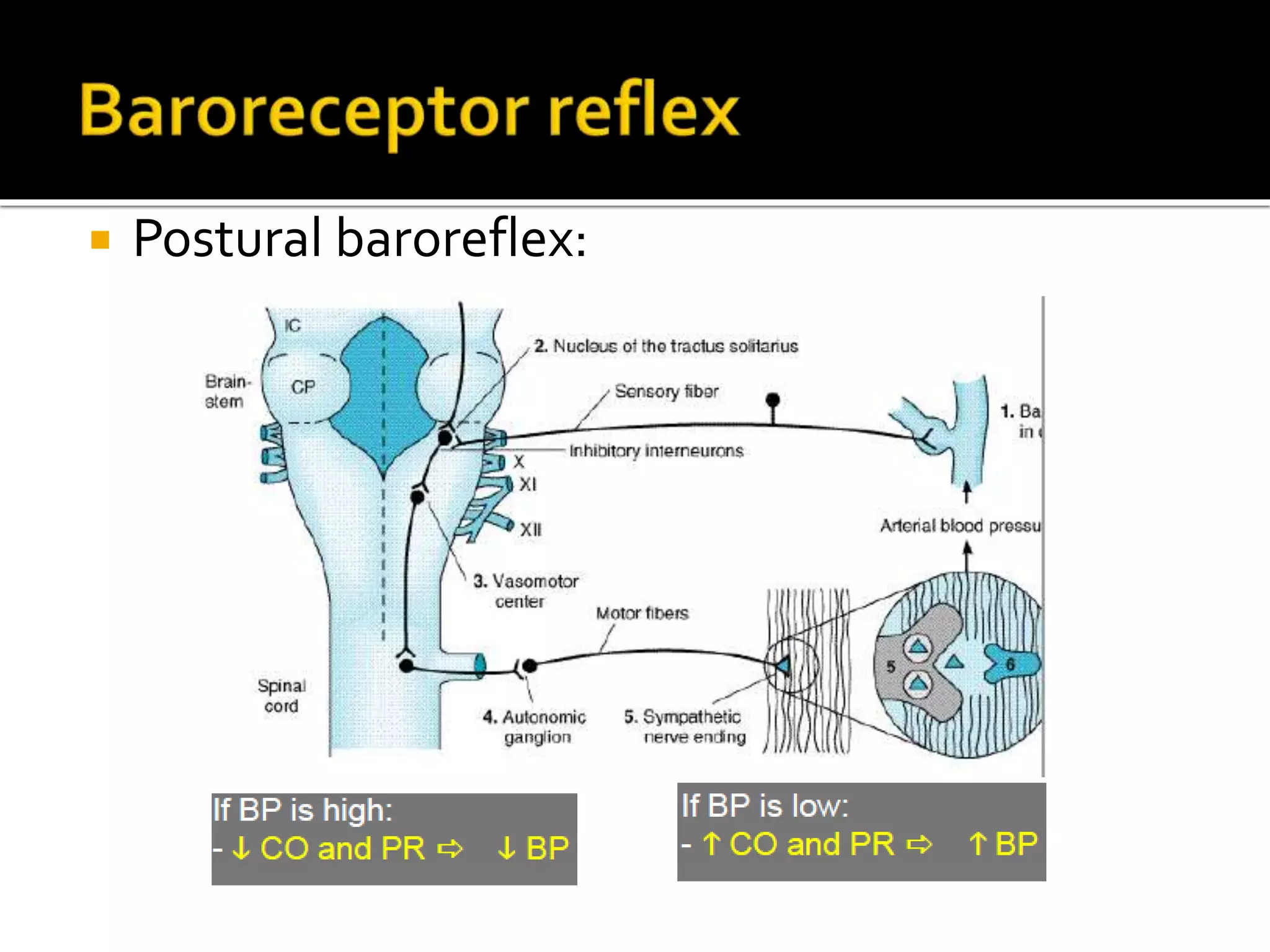
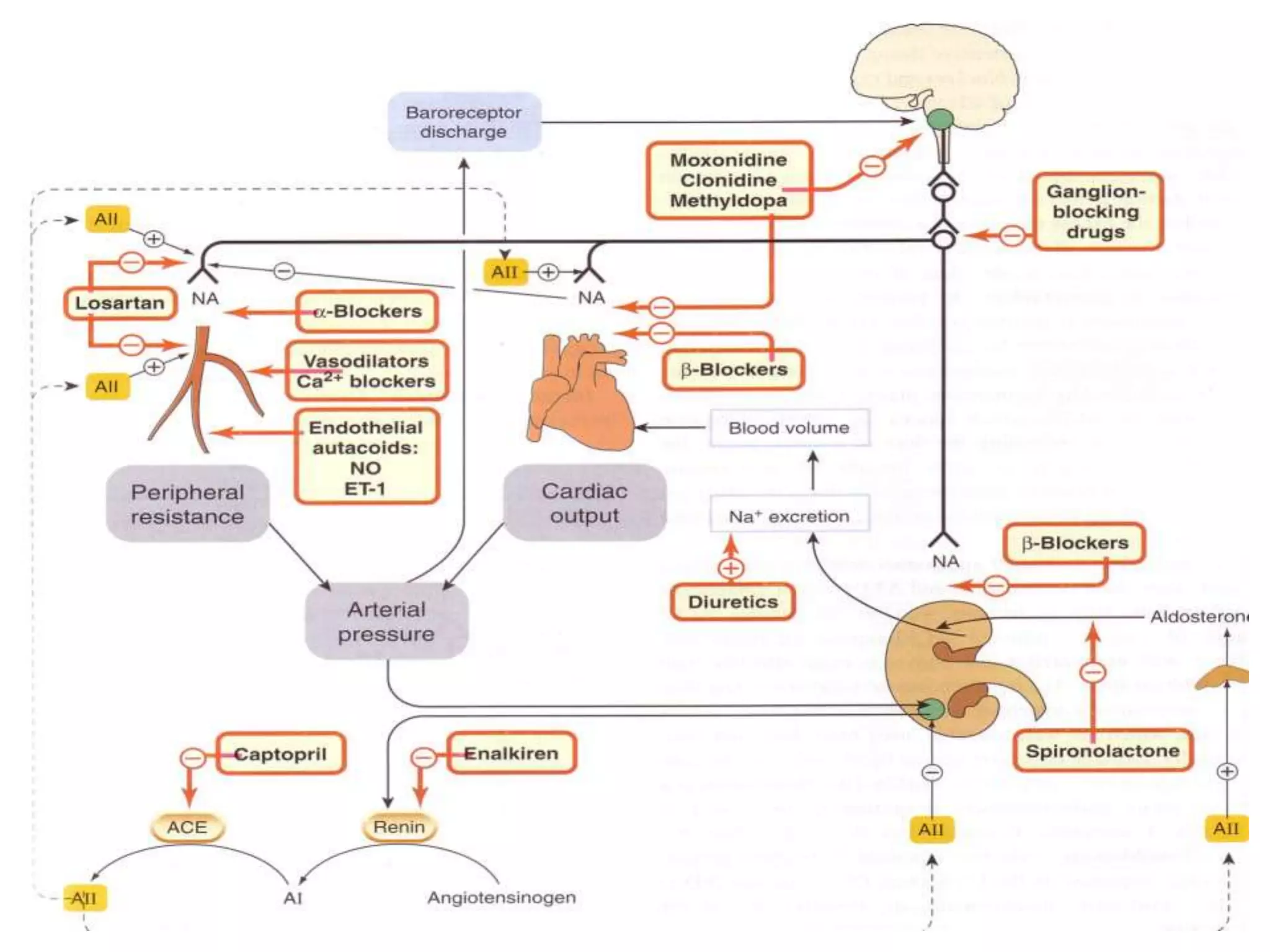
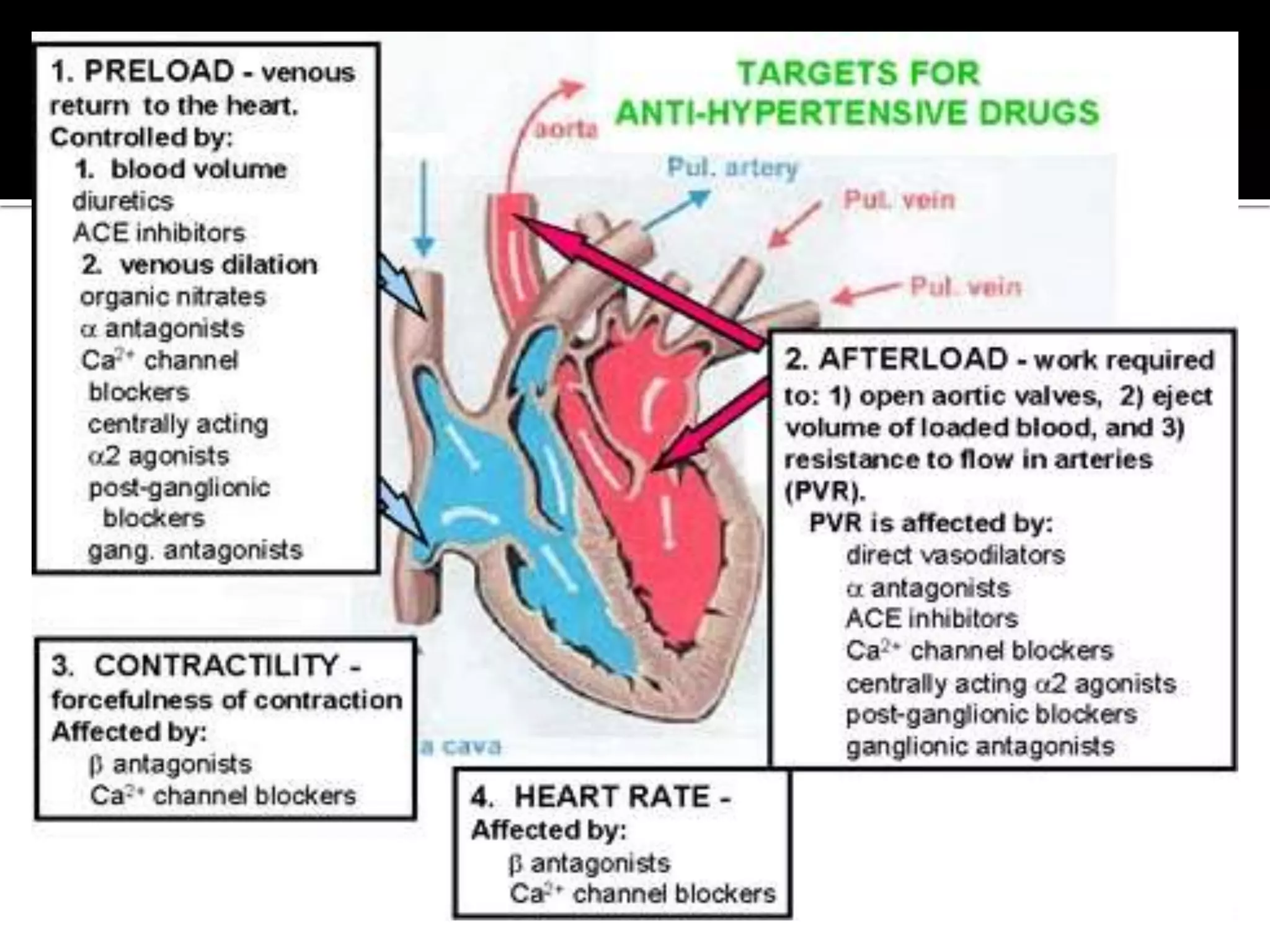
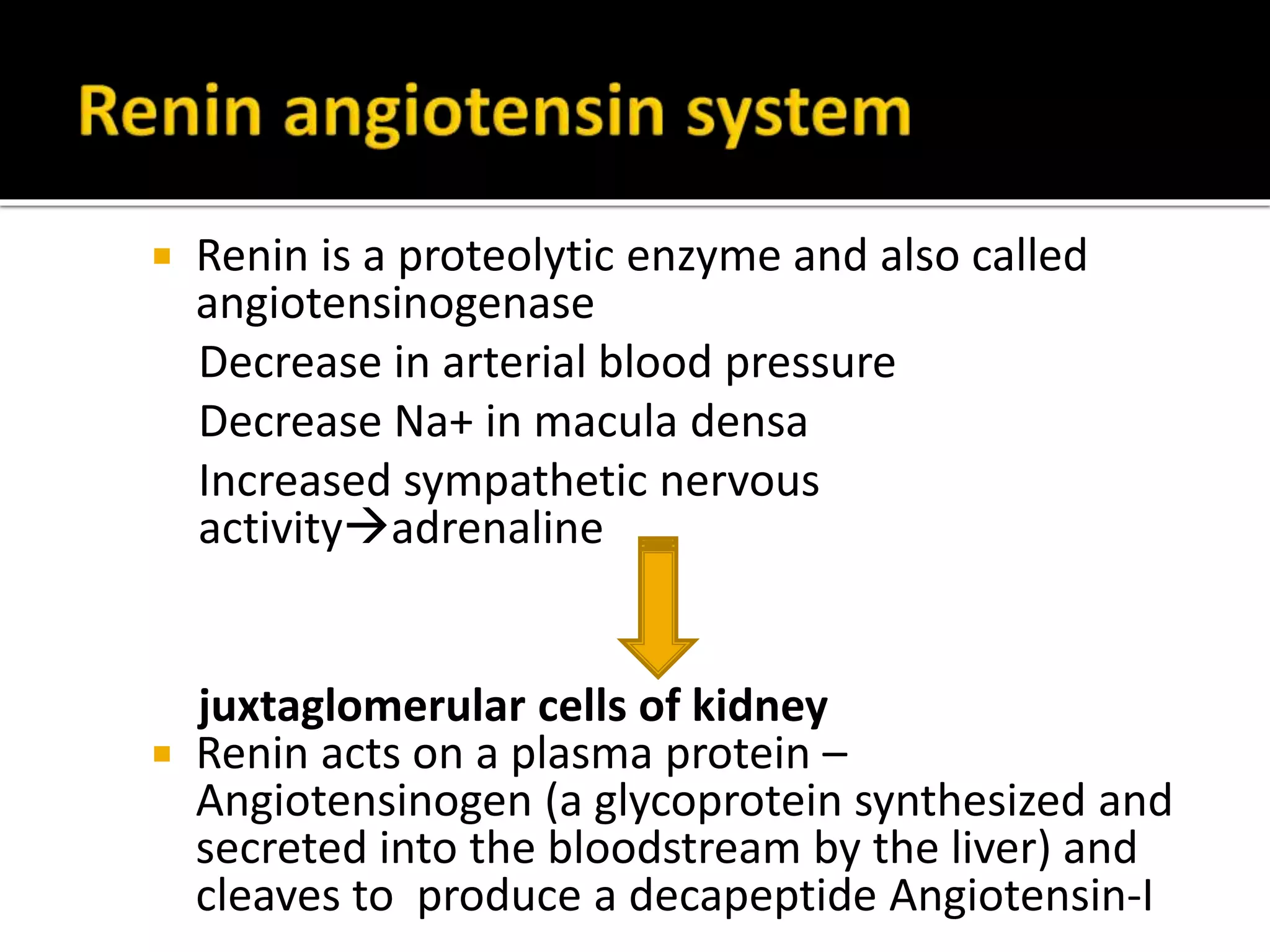
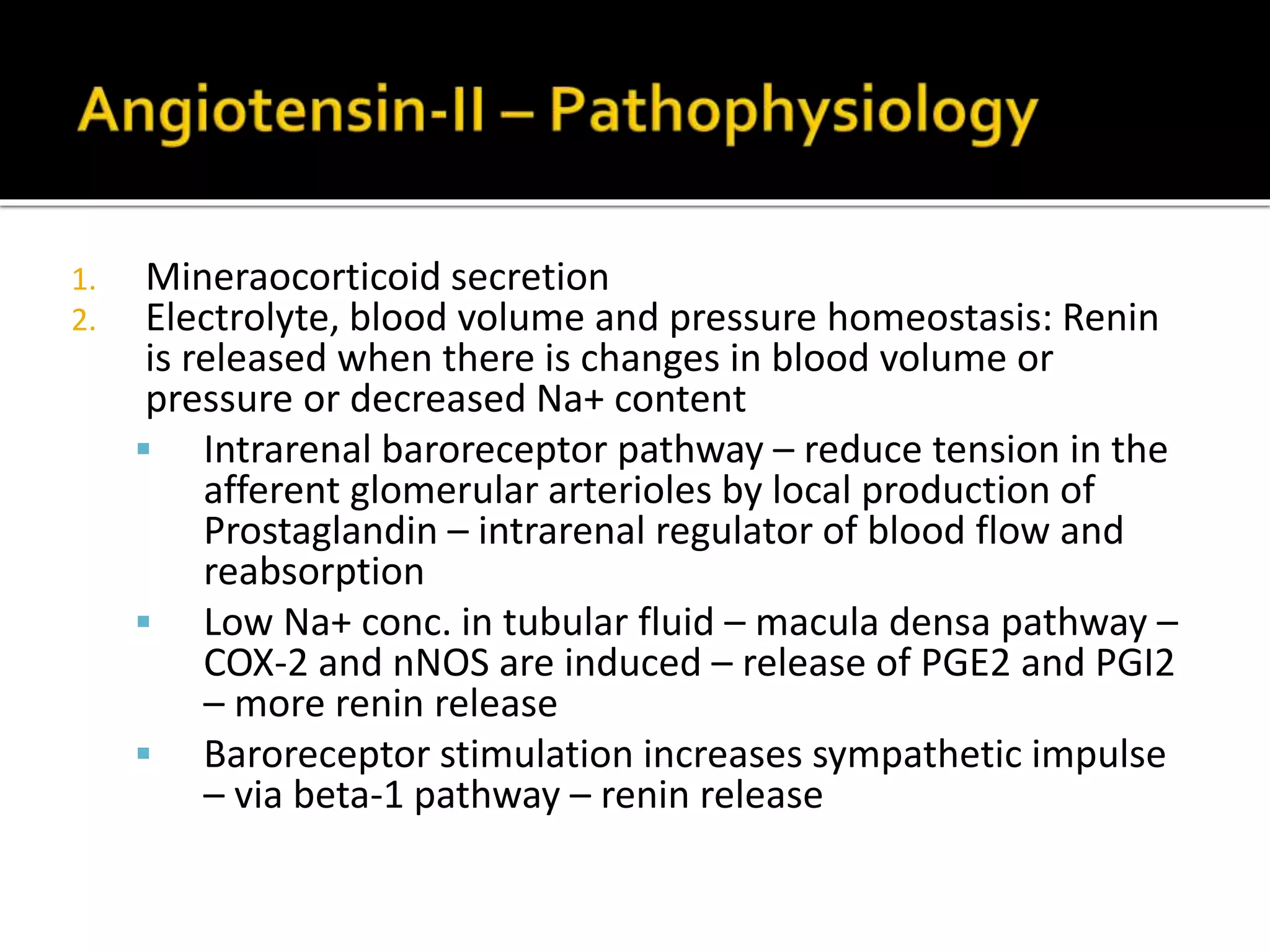
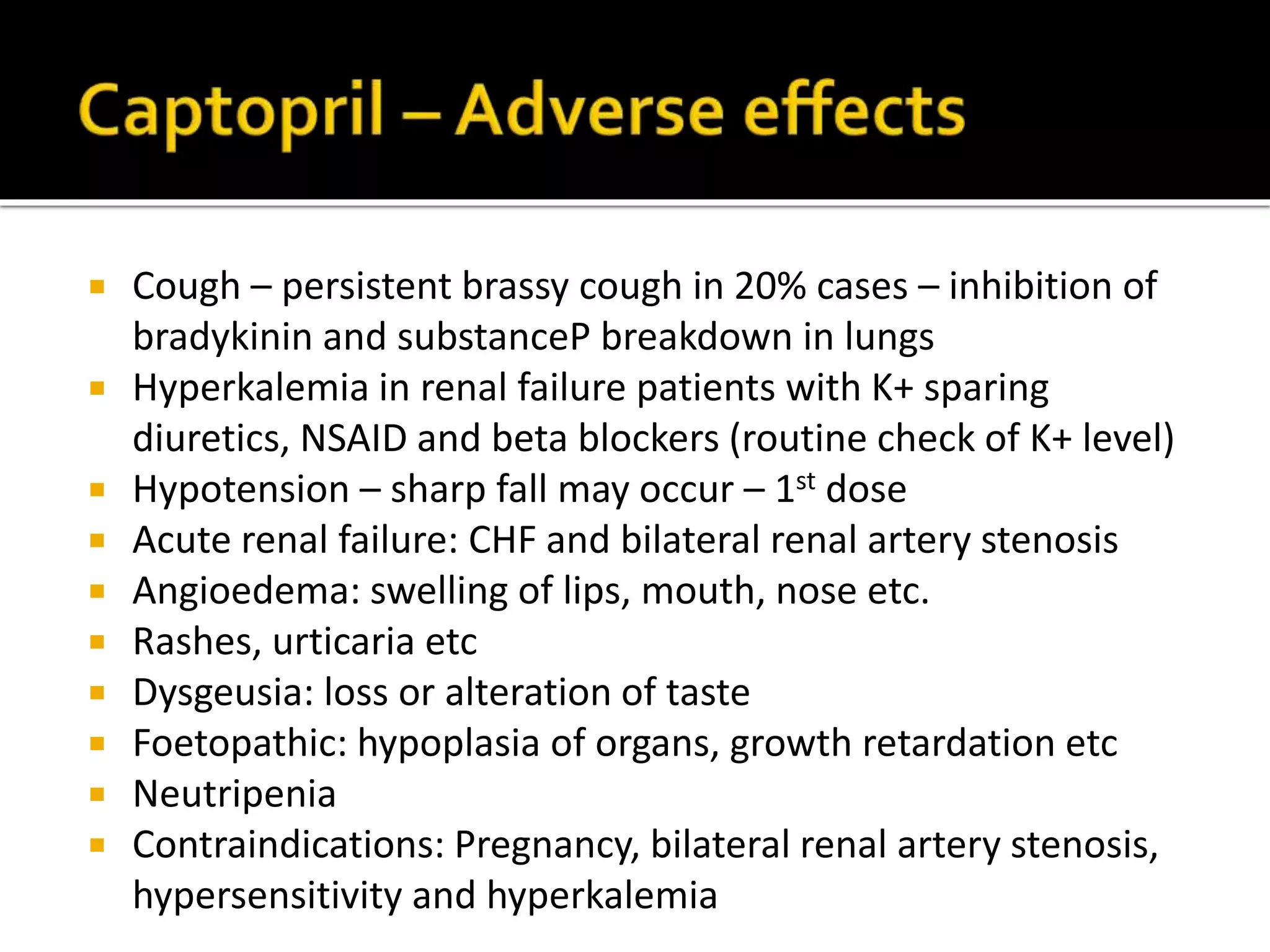
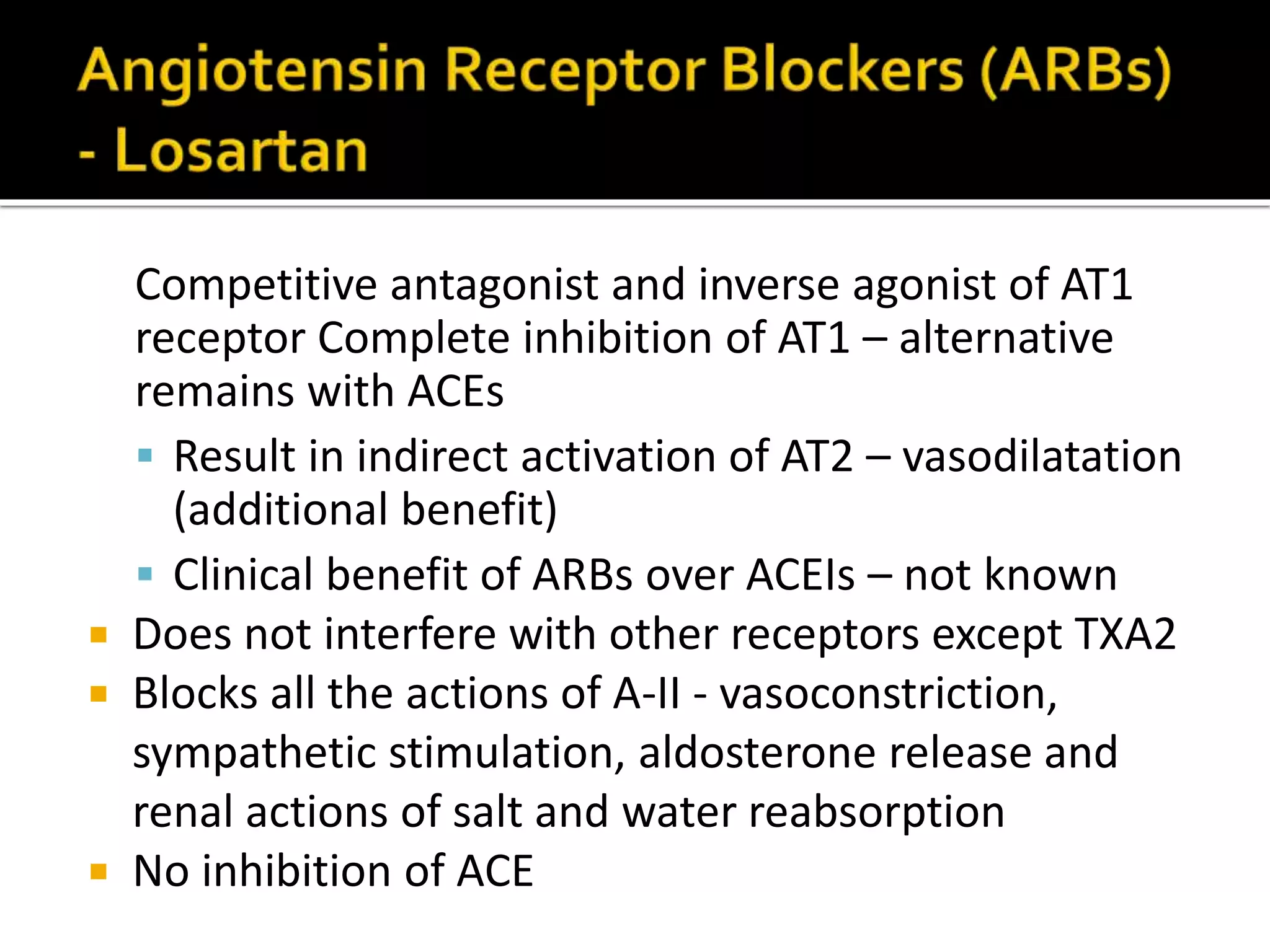
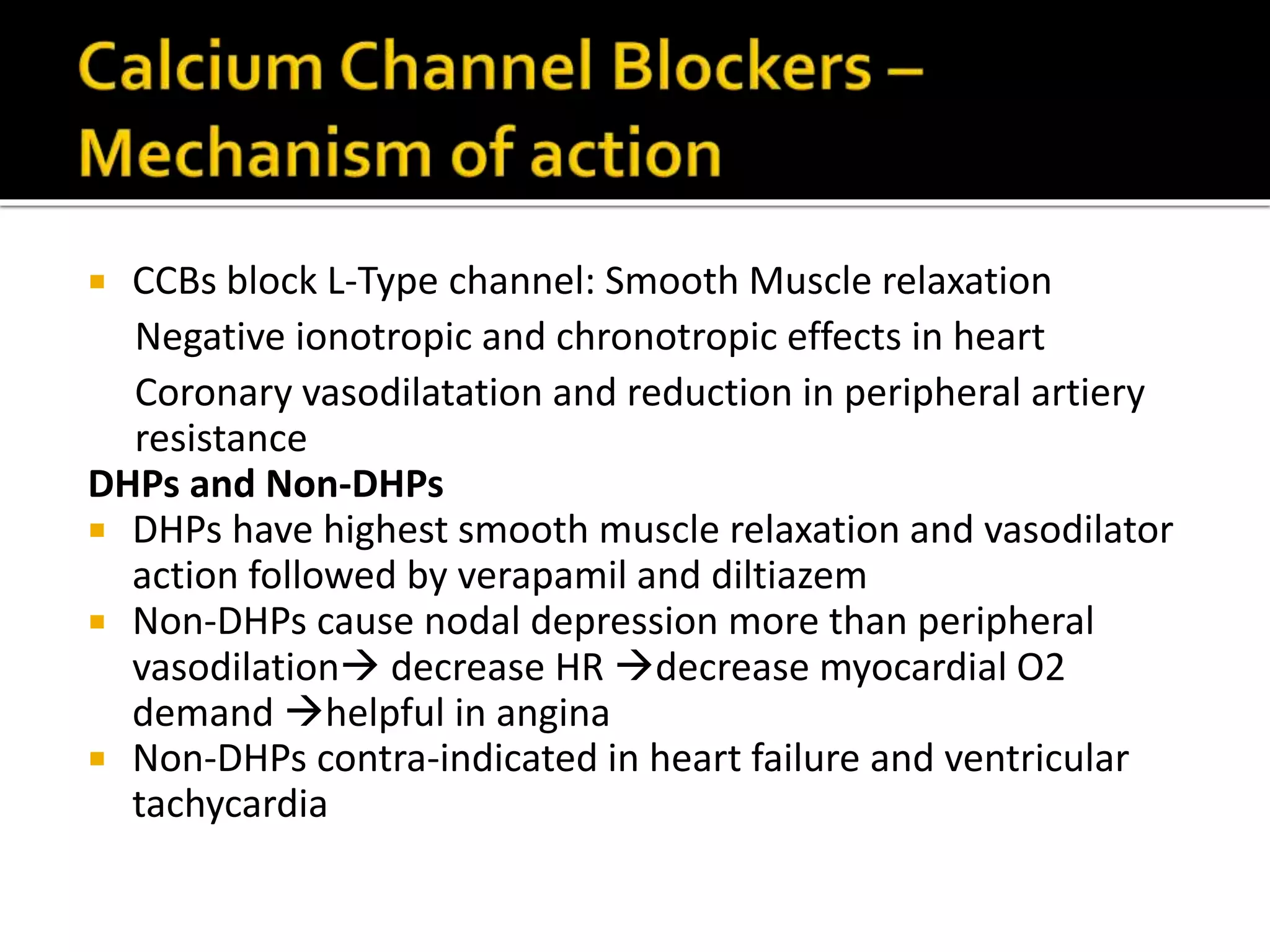
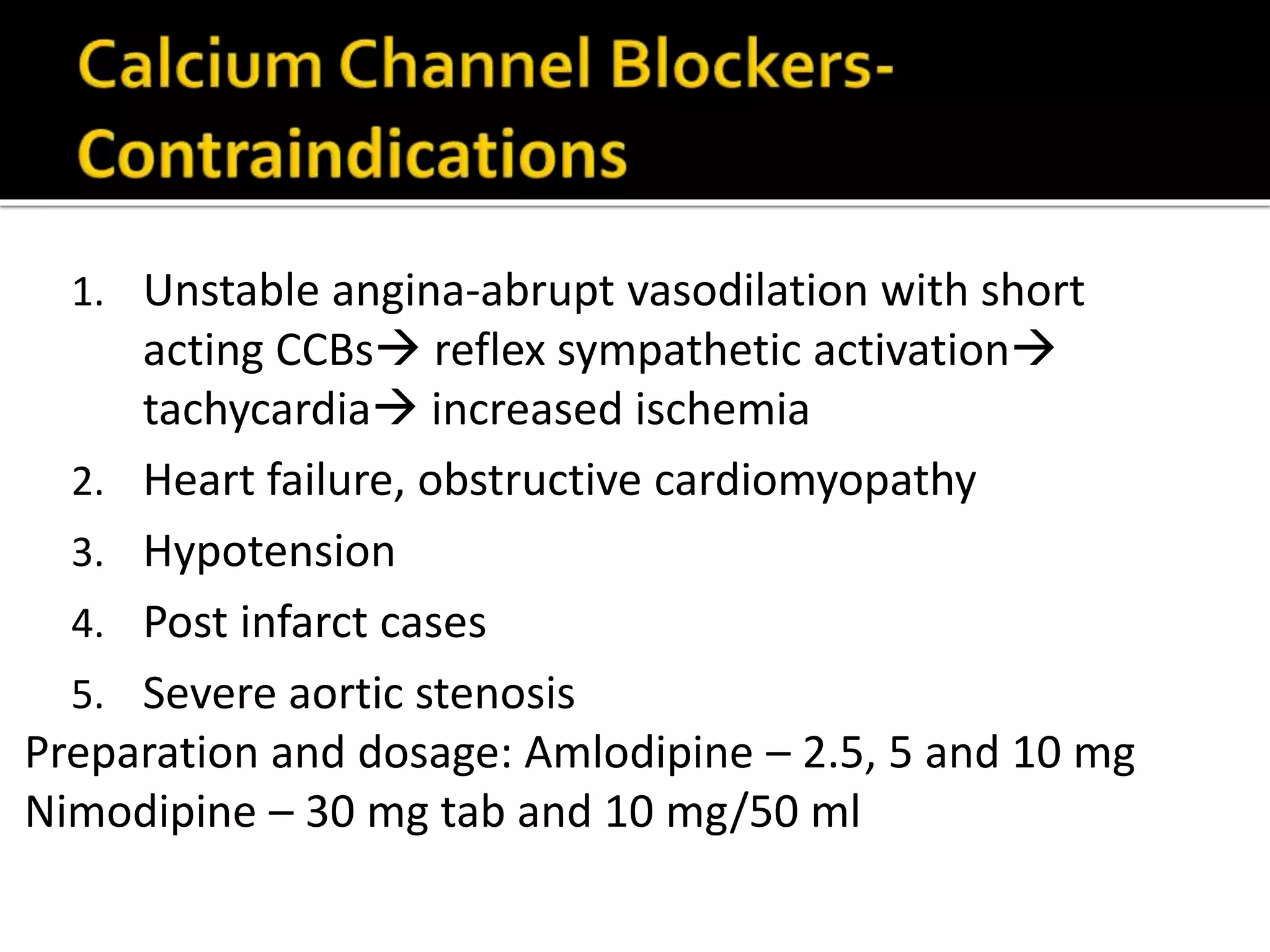
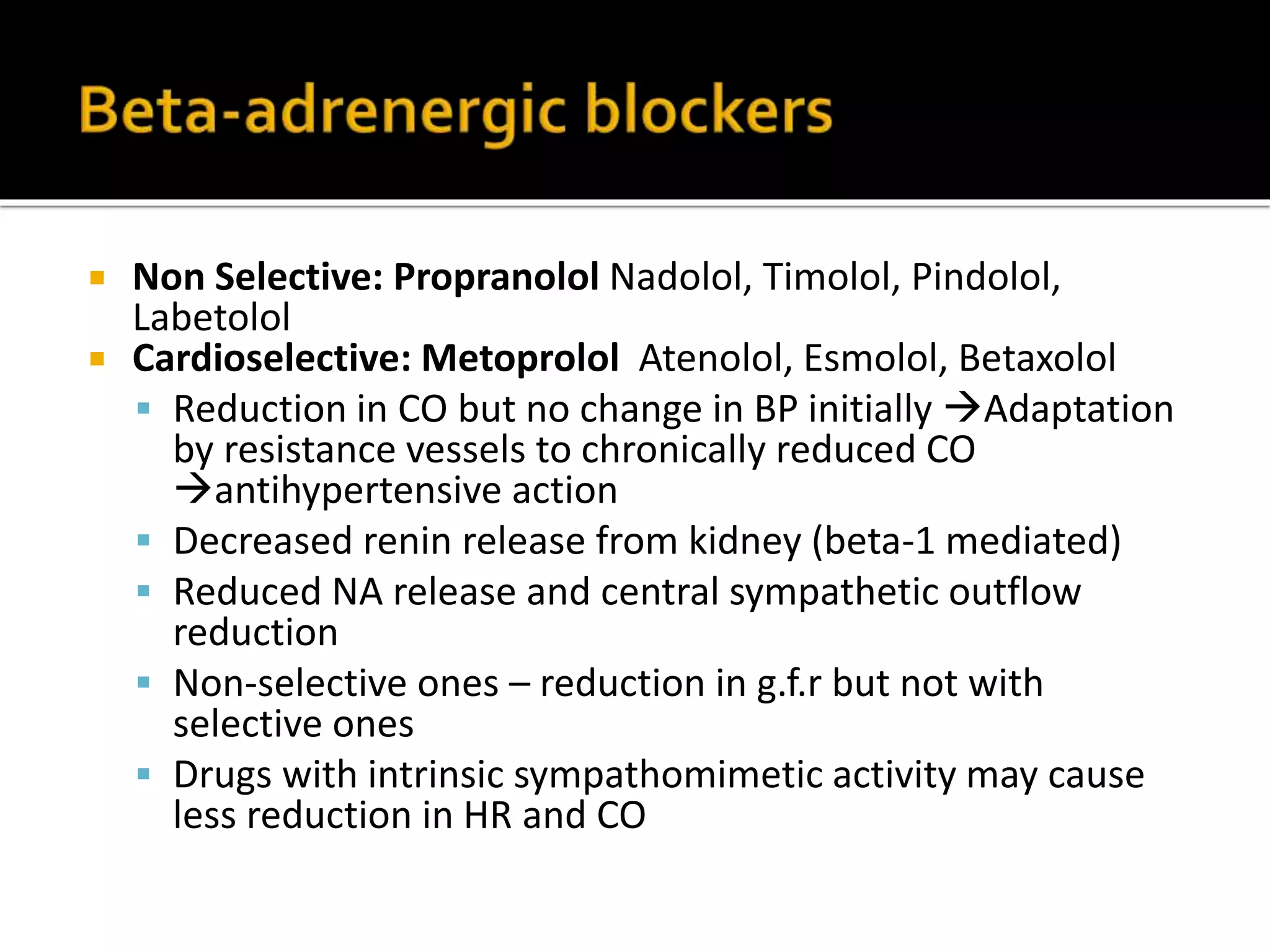
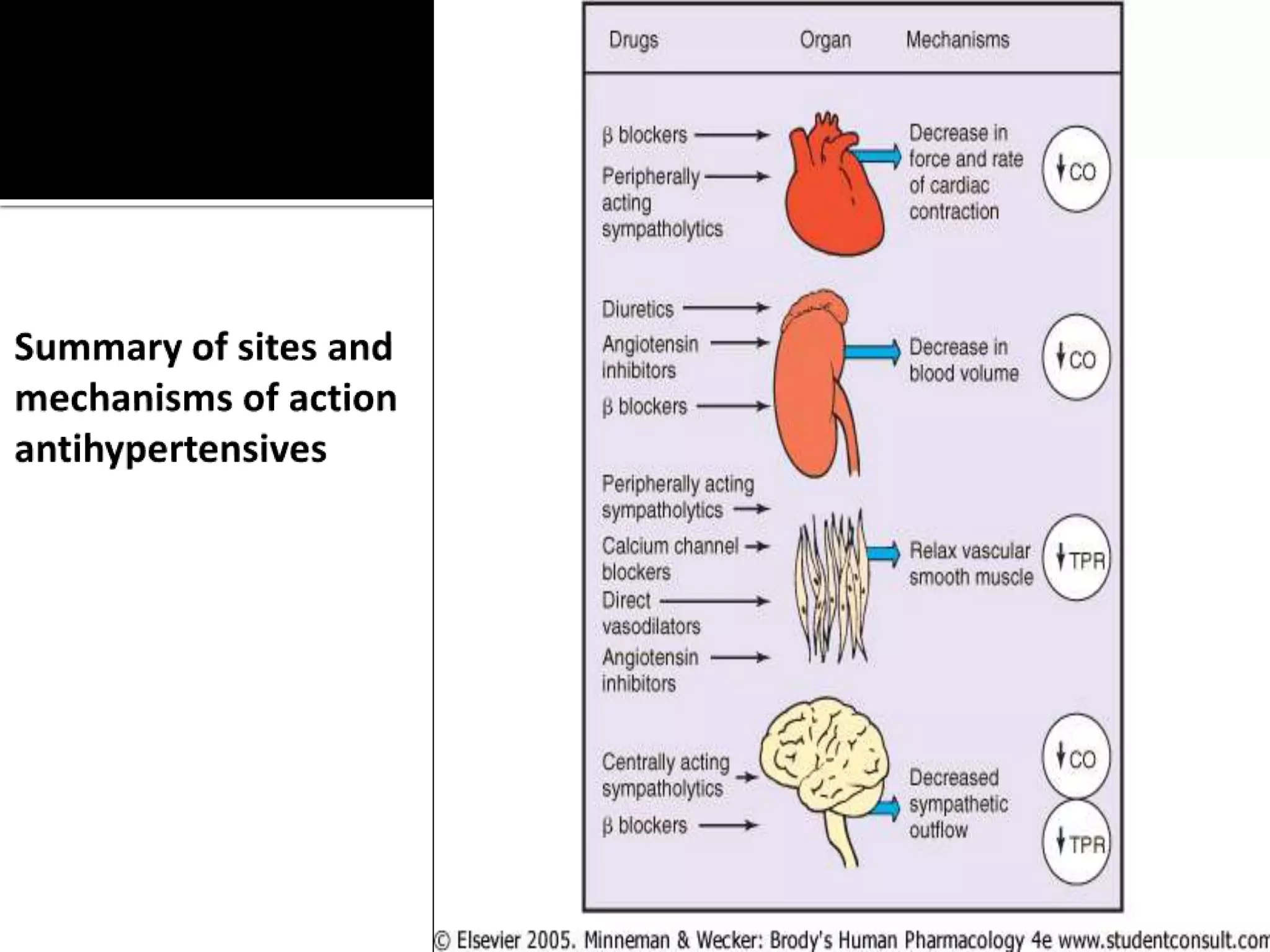
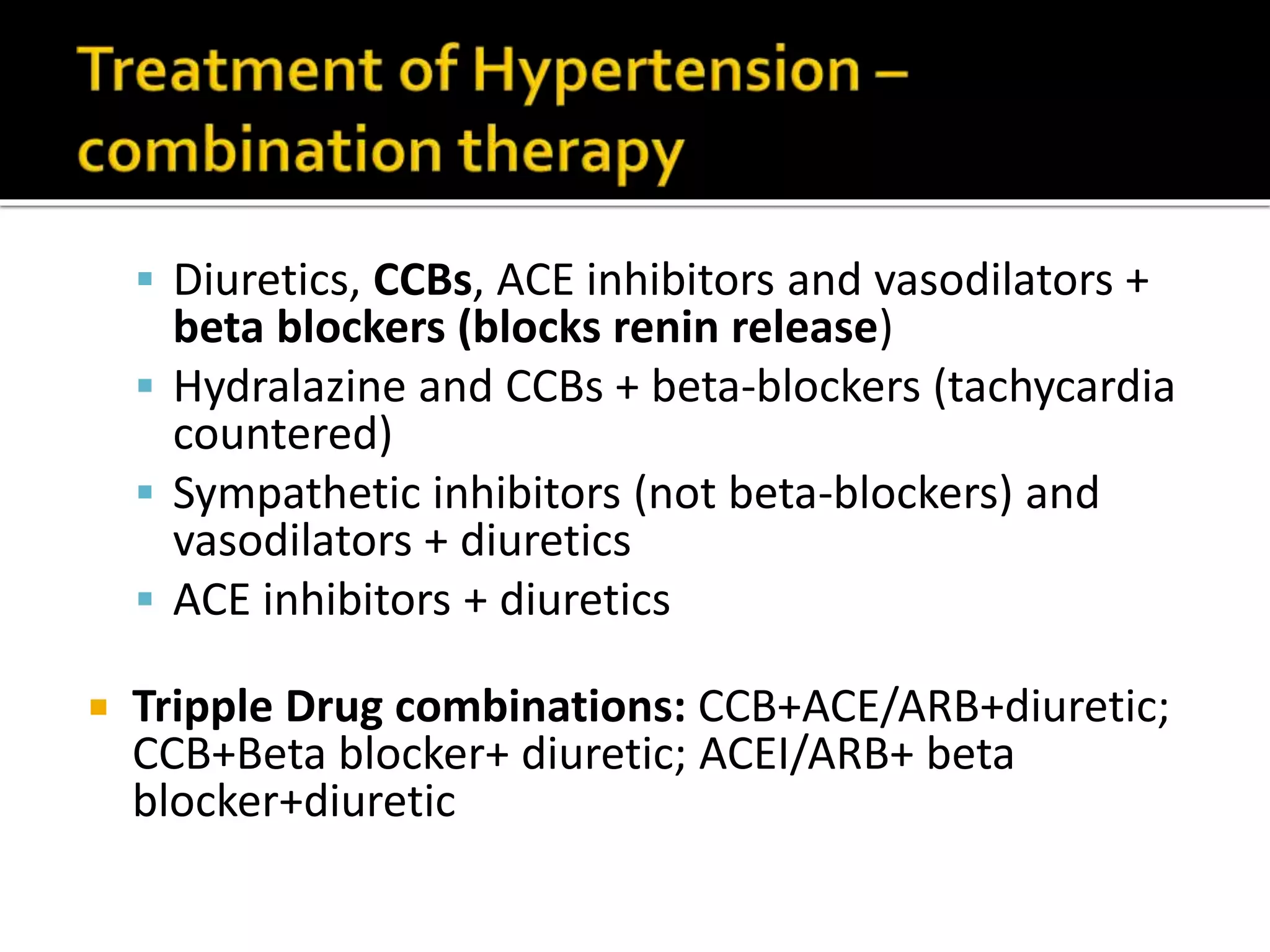
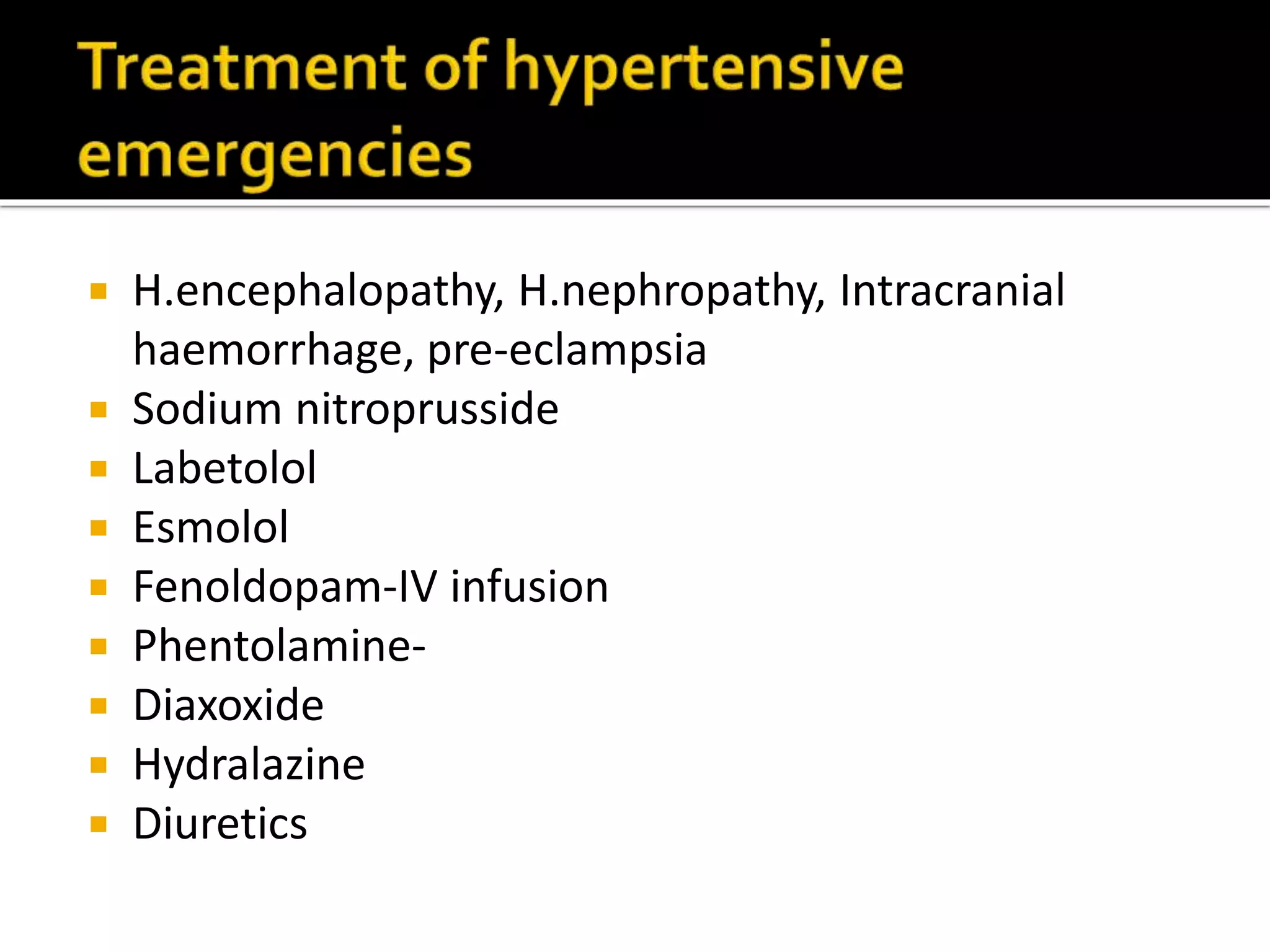
This document discusses various classes of antihypertensive drugs including beta blockers, ACE inhibitors, calcium channel blockers, and diuretics. It explains their mechanisms of action in lowering blood pressure by reducing cardiac output, peripheral resistance, or sodium retention. Some advantages and side effects are provided for each drug class. The renin-angiotensin-aldosterone system and its role in blood pressure regulation is also summarized.