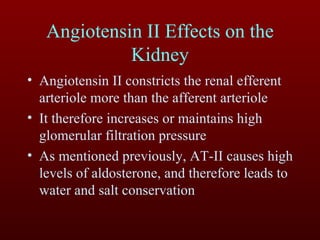
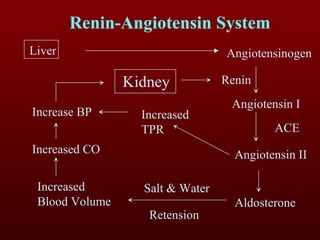
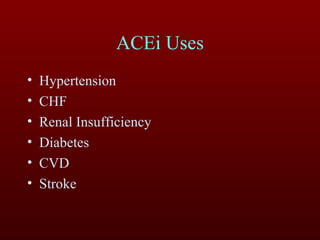
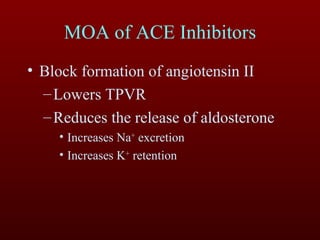
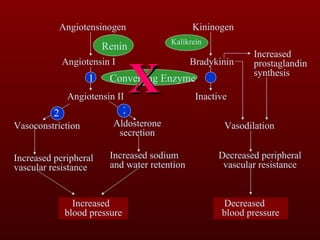
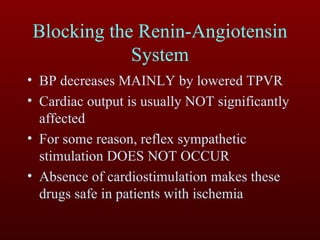
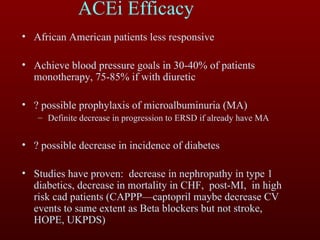
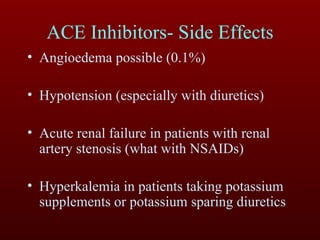
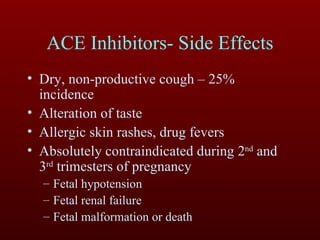
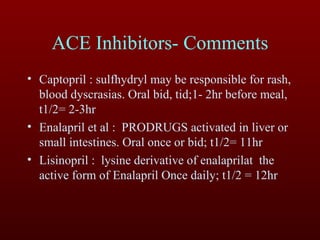
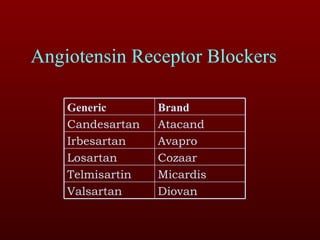
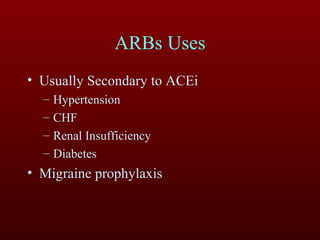
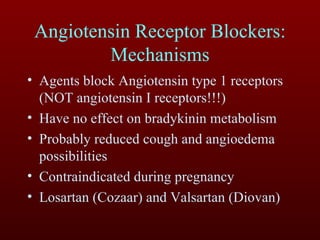
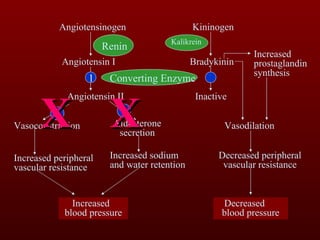
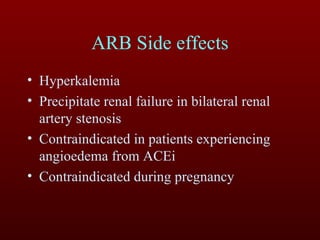
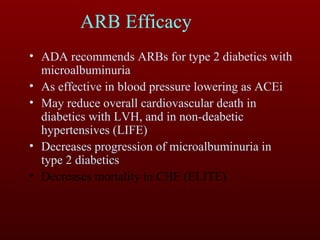
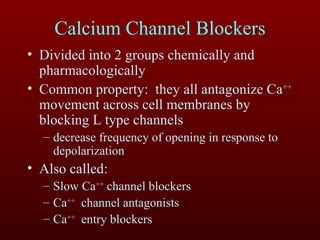
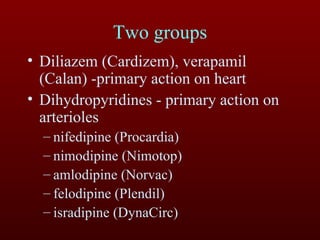
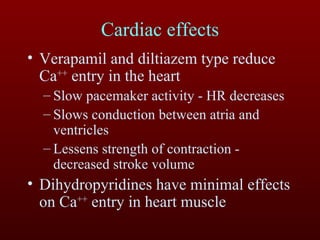
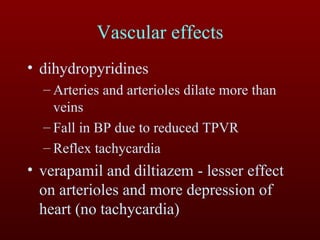
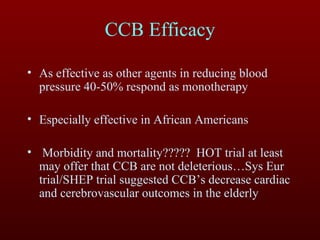
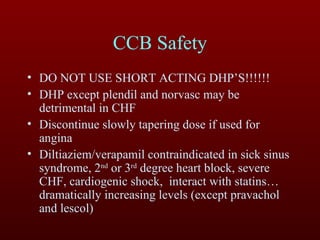
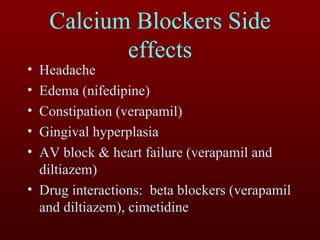
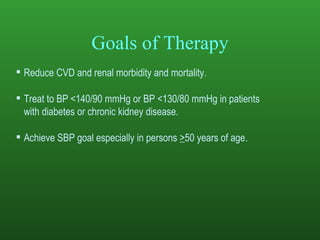
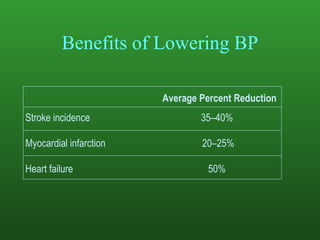
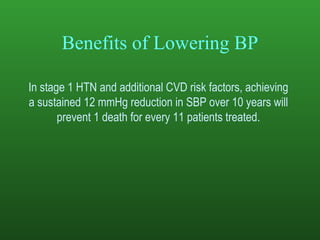
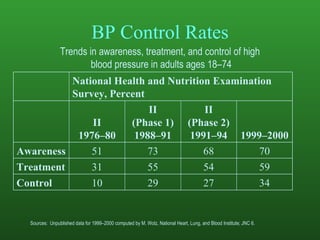
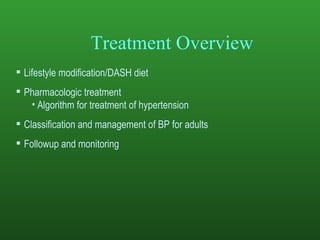
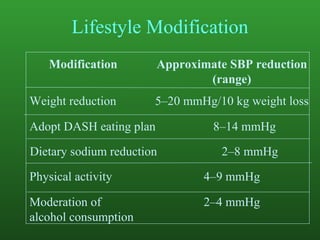
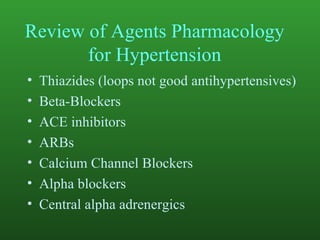
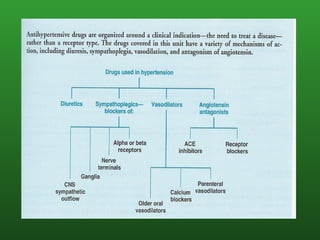
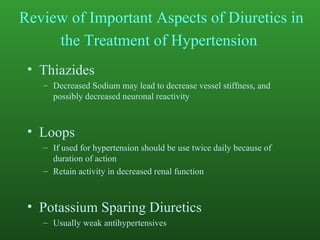
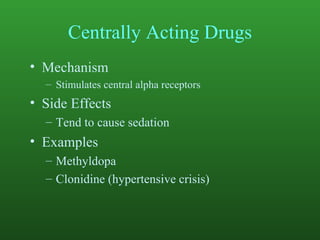
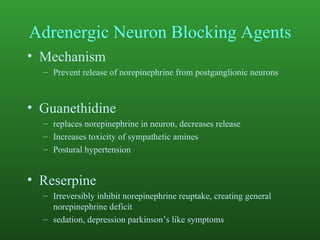
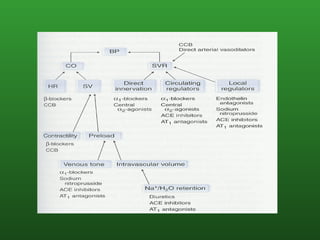
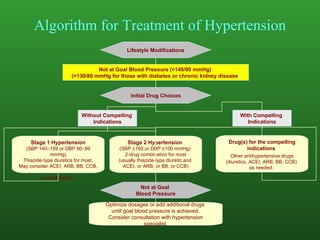
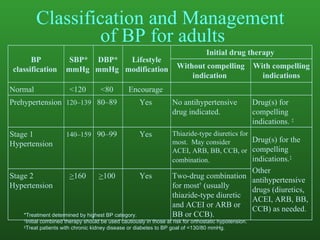
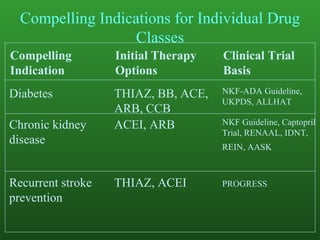
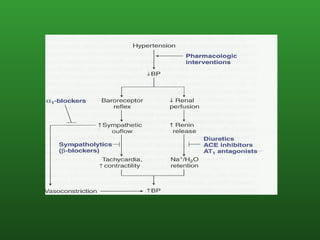
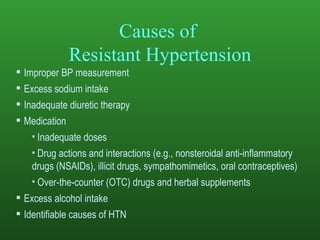
This document summarizes the pharmacology of medications used to treat hypertension, including ACE inhibitors, ARBs, and CCBs. It reviews their mechanisms of action, efficacy, and safety profiles. It also discusses the renin-angiotensin system and its role in hypertension, current treatment guidelines, lifestyle modifications, and algorithms for antihypertensive drug selection and combination therapy.