This document discusses chronic periodontitis, including its characteristics, pathogenesis, clinical presentation, histopathology, and classification. Key points include:
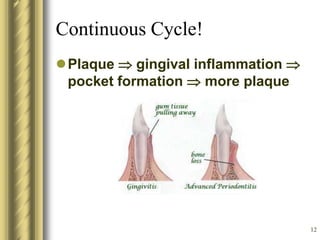
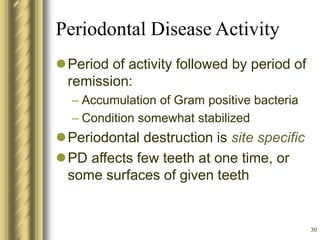
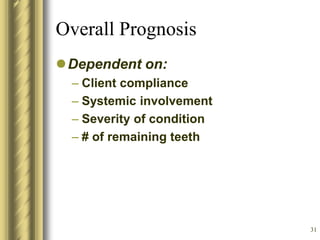
- Chronic periodontitis can be localized or generalized. It typically has an onset in adulthood and is initiated by plaque, with calculus and poor oral hygiene contributing. Progression can be slow or have periods of rapid change, and is modified by local/systemic factors and smoking.
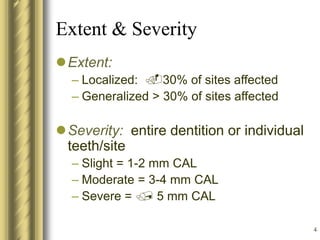
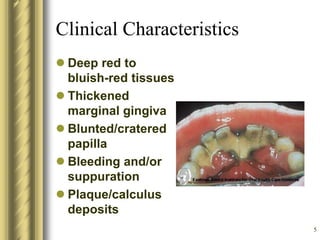
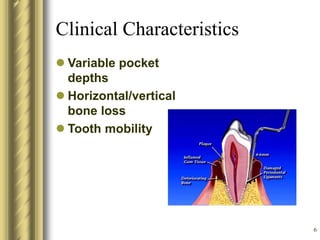
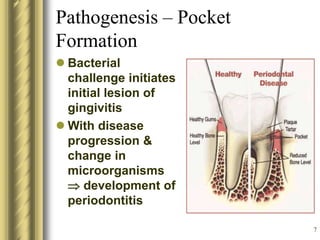
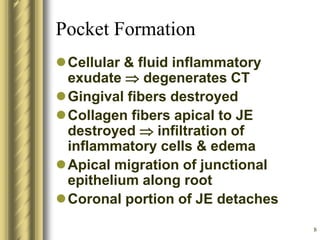
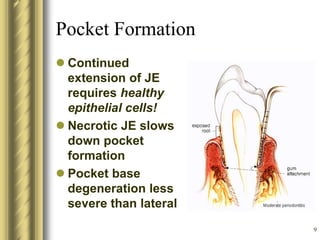
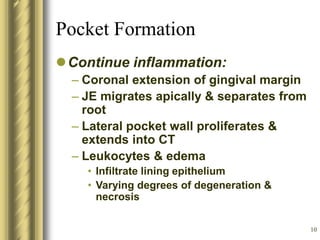
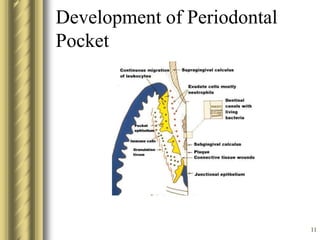
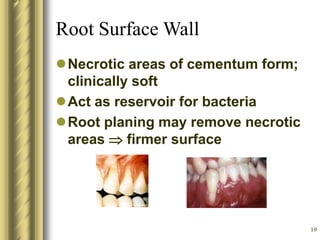
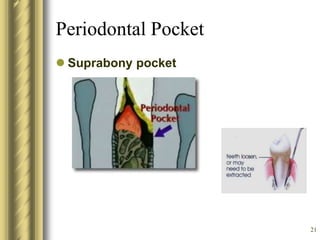
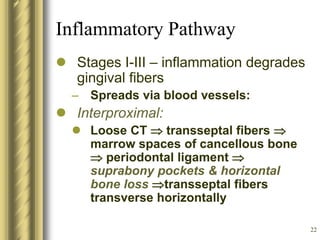
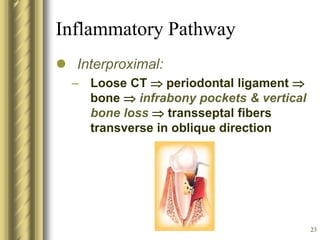
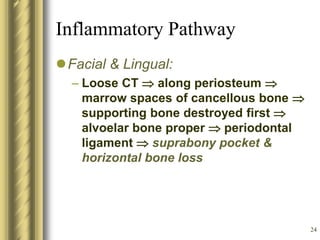
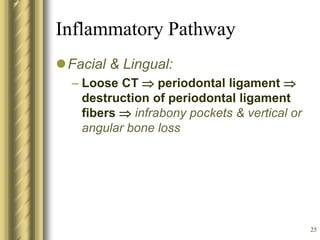
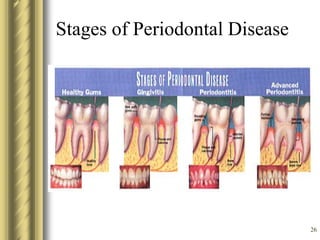
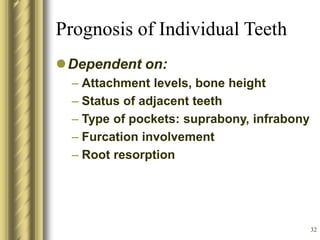
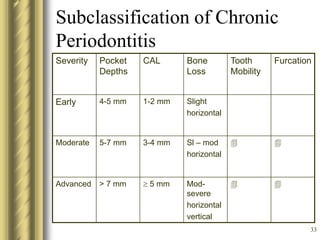
- The extent and severity are classified based on the percentage of sites affected and amount of clinical attachment level (CAL) loss/bone loss. Pockets form from bacterial challenge causing gingival inflammation and destruction of connective tissue fibers.
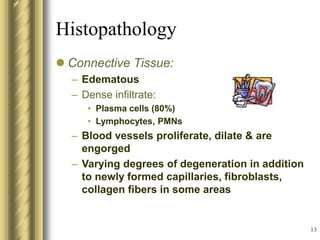
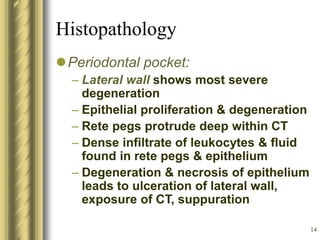
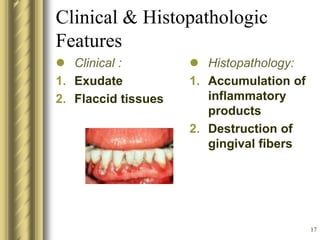
- Histopathology shows