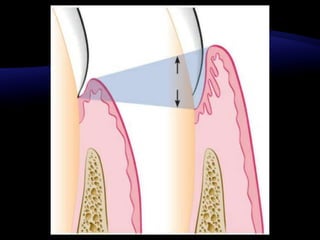
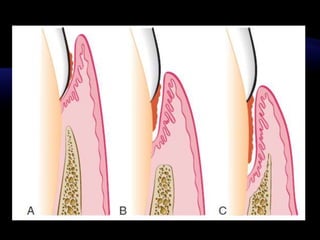
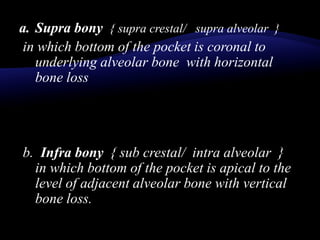
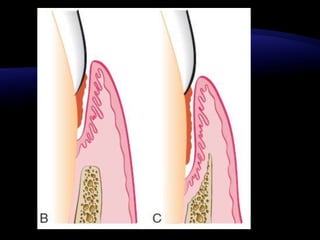
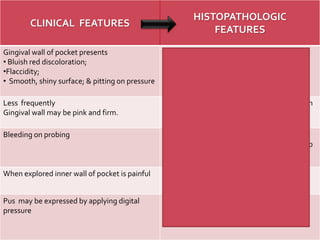
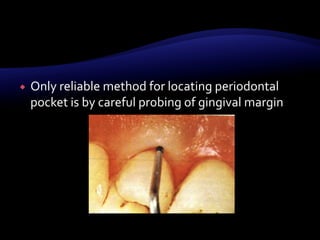
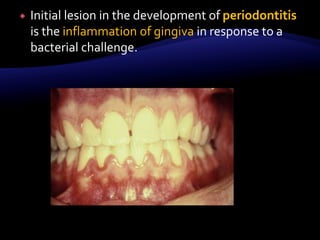
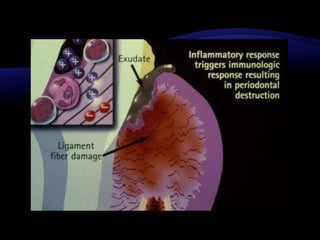
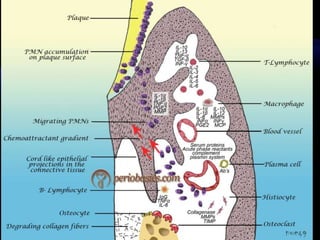
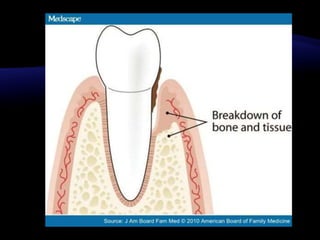
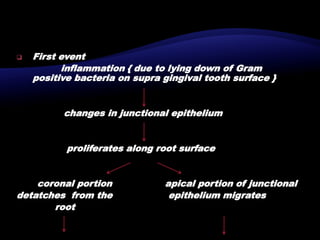
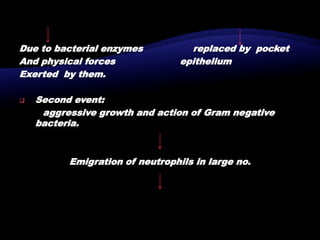
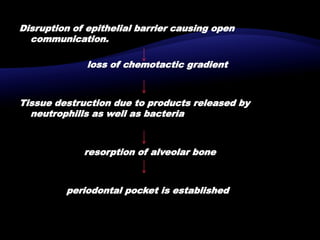
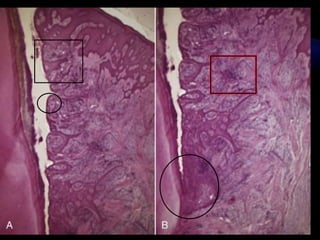
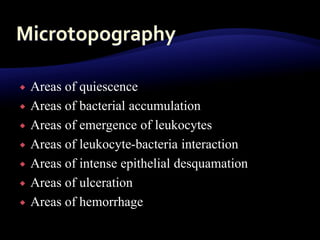
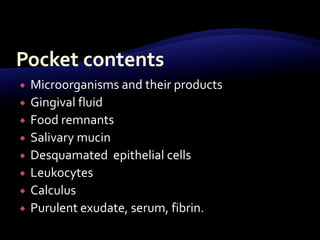
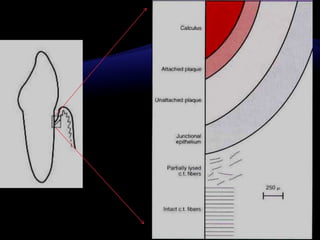
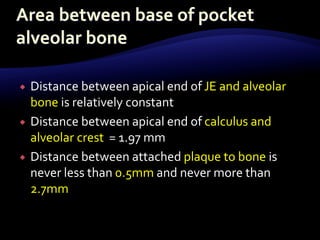
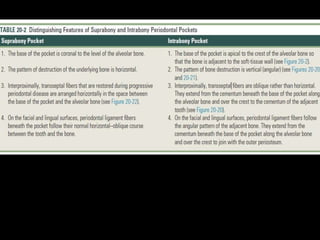
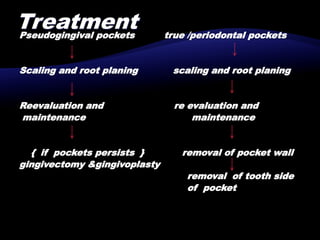
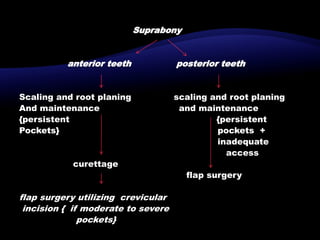
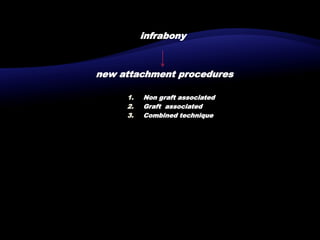
This document discusses the classification, clinical features, and histopathology of periodontal pockets. It classifies pockets as gingival/pseudo pockets or true periodontal pockets. Periodontal pockets are further classified based on their location relative to the alveolar bone as supra bony or infra bony. The clinical features include signs like thickened gingiva and bleeding on probing. Histopathologically, the soft tissue wall shows increased blood vessels and plasma cells, while the root surface shows changes like pathologic granules and mineralization/demineralization. Treatment involves scaling and root planing, with surgery for persistent deep pockets.