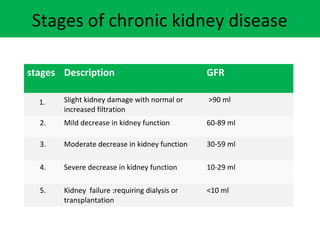
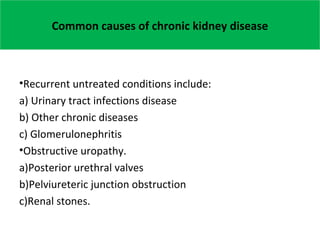
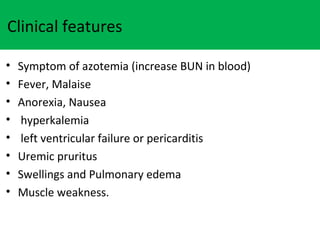
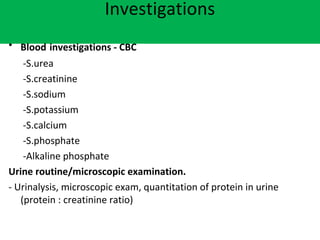
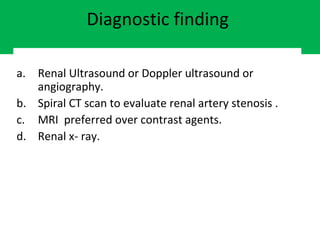
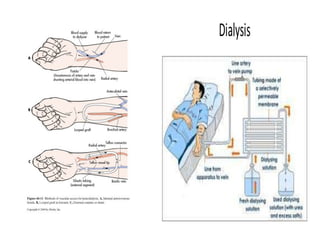
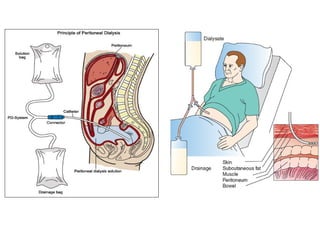
This document discusses chronic kidney disease and end stage renal disease. It defines chronic kidney disease as kidney damage or decreased glomerular filtration rate for more than 3 months. It describes the 5 stages of chronic kidney disease based on GFR level. Common causes include infections, diseases like glomerulonephritis, obstructive issues, developmental anomalies, and genetic factors. End stage renal disease requires renal replacement therapy like hemodialysis, peritoneal dialysis, or kidney transplantation. The document outlines considerations for each treatment approach and notes nursing diagnoses and management strategies for patients with chronic kidney failure.