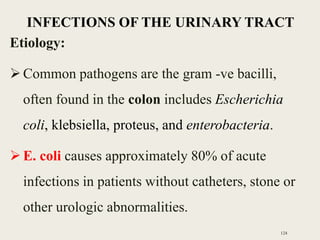
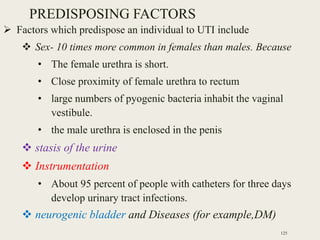
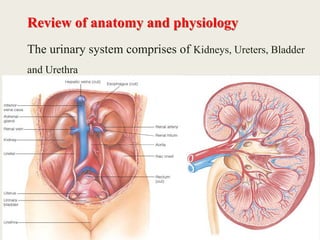
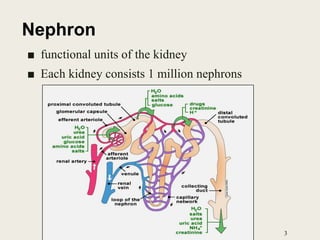
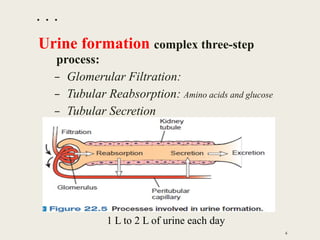
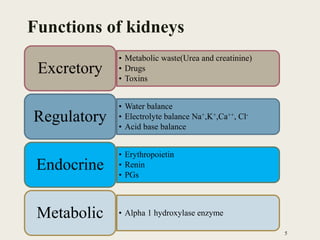
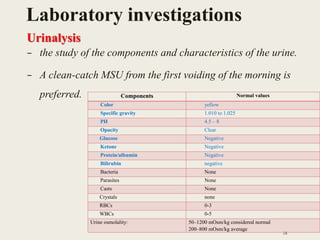
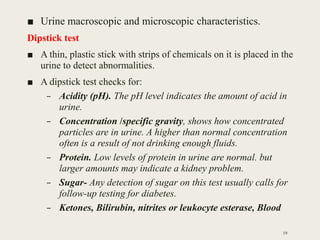
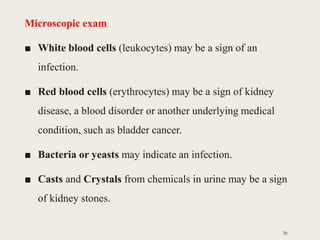
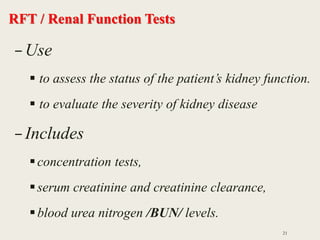
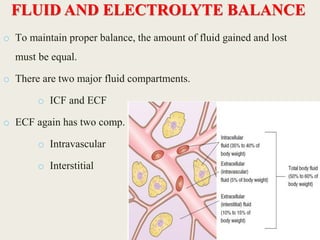
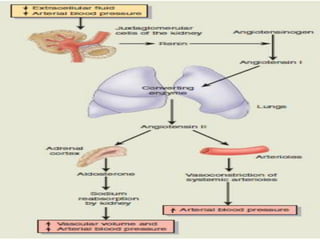
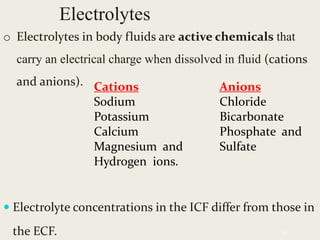
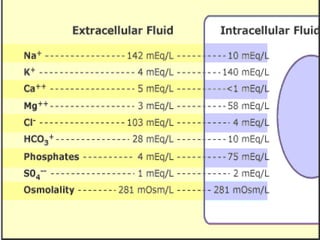
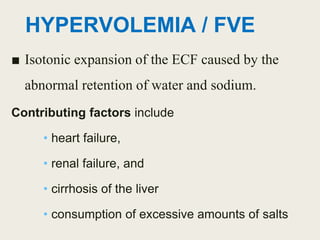
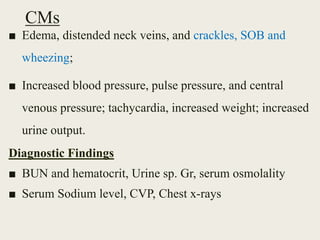
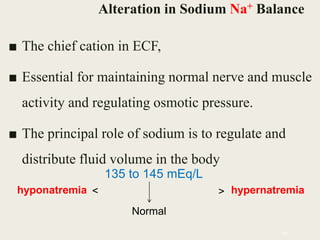
This document provides an overview of nursing interventions for patients with genitourinary disorders. It begins with a review of kidney anatomy and physiology, including nephron structure and urine formation processes. Common tests for assessing kidney function are outlined, such as renal function tests, urinalysis, and diagnostic imaging. Electrolyte and fluid imbalances like hypovolemia, hypervolemia, hyponatremia, and hypernatremia are described along with their causes, signs/symptoms, diagnostic findings, and medical management. Nursing diagnoses and interventions are also mentioned for maintaining fluid and electrolyte balance in patients with genitourinary issues.
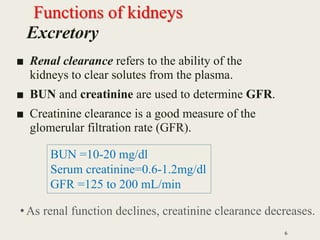
![BUN / Blood Urea Nitrogen
■ Urea is nitrogenous end product of protein
metabolism.
■ Serves as index of renal function.
■ Test values are affected by protein intake, tissue
breakdown, and fluid volume changes.
■ Rises when renal function deteriorates.
27
Blood urea nitrogen [BUN: 10–20 mg/dl]](https://image.slidesharecdn.com/genitourinarynursing-171101125527/85/Genitourinary-nursing-27-320.jpg)
![SODIUM EXCESS (Hypernatremia)
■ > 145 mEq/L [145 mmol/L])
■ Can be caused by
– a gain of sodium in excess of water or
– a loss of water in excess of sodium.
■ It can be associated with FVD or FVE.
Causes
– Administration of hypertonic enteral feedings without
adequate water
– watery diarrhea and greatly increased insensible water
loss (hyperventilation, Increased sweating)
– Diabetes insipidus, a deficiency of ADH
52](https://image.slidesharecdn.com/genitourinarynursing-171101125527/85/Genitourinary-nursing-52-320.jpg)
![Medical Management
■ Gradual lowering of the serum sodium level
hypotonic solution (eg, 0.3% NaCl) thereby
decreases the risk of cerebral edema
–Isotonic nonsaline solution (eg, dextrose 5% in
water [D5W]).
Nursing Management
■ I/O, Diuretics
■ obtain a medication history because some
prescription medications have a high sodium
content
■ monitor for changes in behavior
54](https://image.slidesharecdn.com/genitourinarynursing-171101125527/85/Genitourinary-nursing-54-320.jpg)