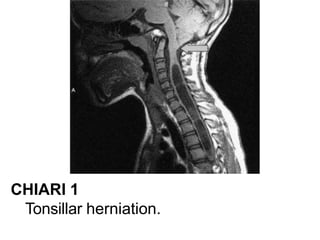
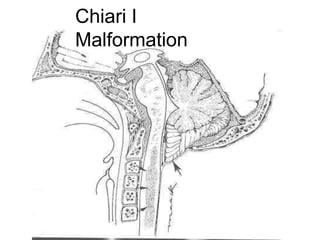
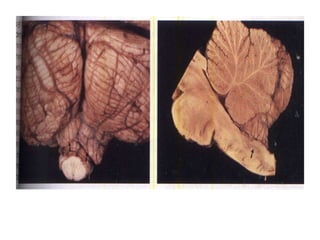
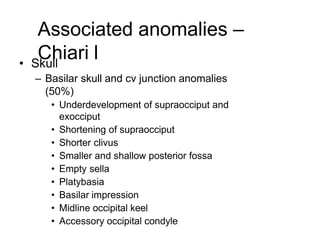
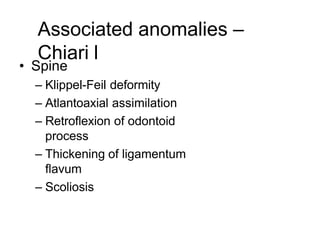
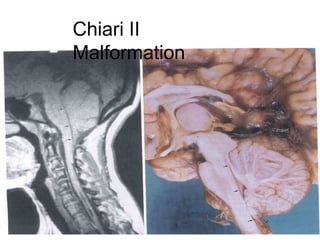
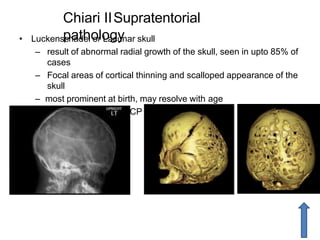
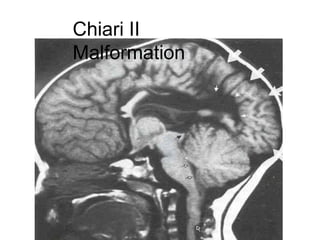
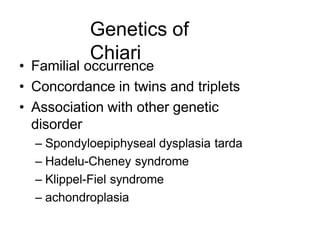
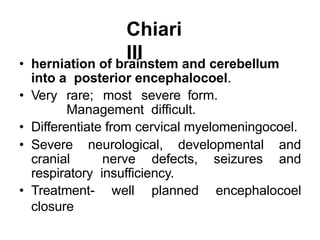
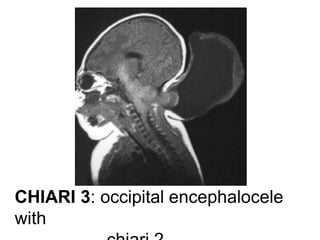
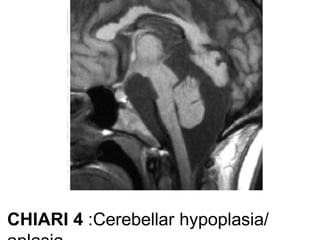
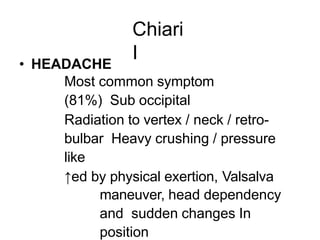
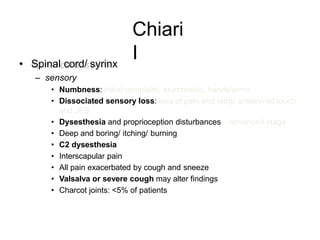
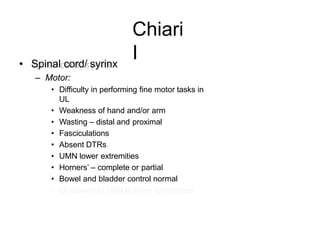
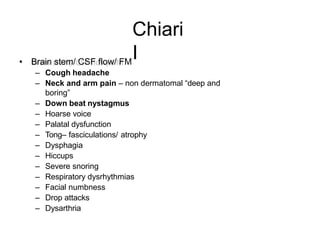
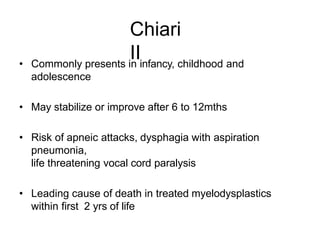
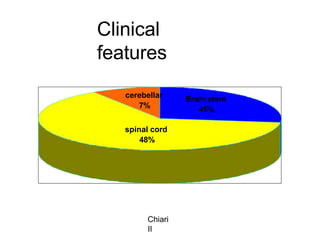
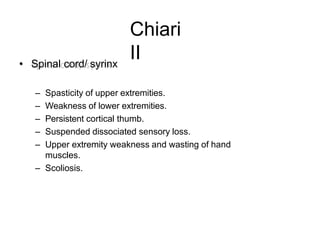
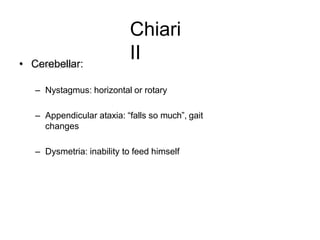
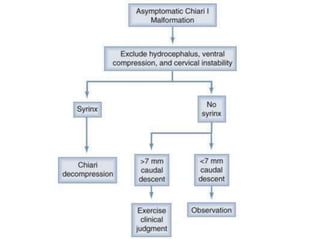
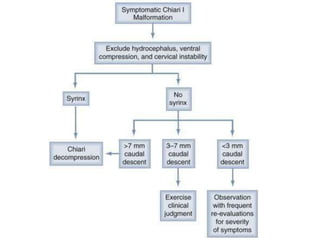
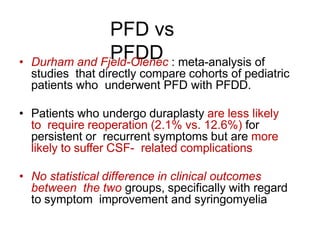
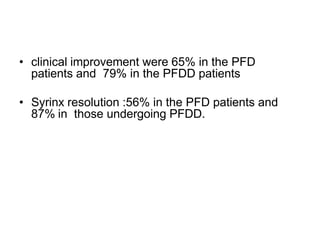
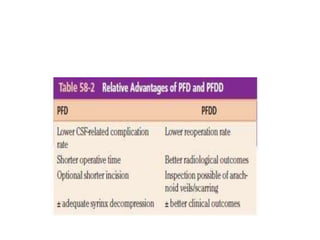
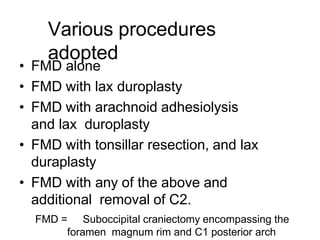
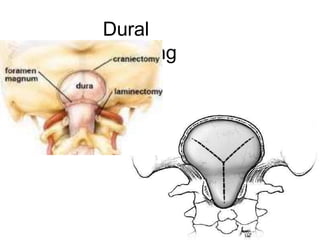
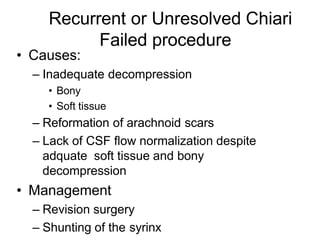
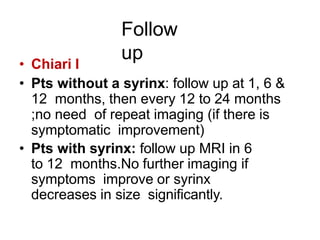
Chiari malformations are a group of hindbrain abnormalities classified into four types, ranging from Chiari I with tonsillar herniation to Chiari IV characterized by cerebellar hypoplasia. The document discusses associated anomalies, clinical features, and management approaches for each type, emphasizing diagnostic imaging and surgical interventions for symptomatic patients. Key considerations for surgical procedures include tonsillar descent, the presence of syrinx, and potential postoperative complications.