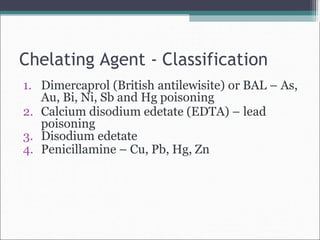
This document discusses chelating agents, which are compounds that bind to heavy metals to form stable complexes that can be safely eliminated from the body. Chelating agents contain functional groups like hydroxyl, carboxyl, amino or phosphate that bind metals. They work by competing with biomolecules in the body for heavy metals, preventing toxicity. An ideal chelating agent strongly binds toxic metals while having less affinity for essential metals. Some chelating agents discussed include dimercaprol (BAL), which treats arsenic, mercury and other metal poisonings; penicillamine for copper and lead poisoning; and calcium disodium edetate for lead poisoning. Desferrioxamine is used to treat acute iron poisoning by binding iron