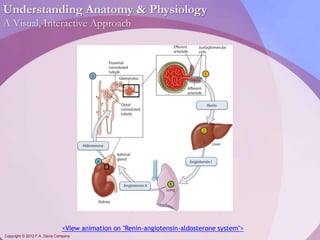
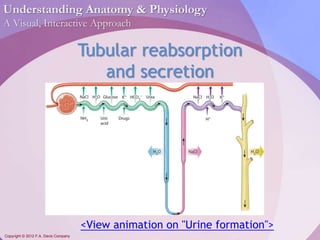
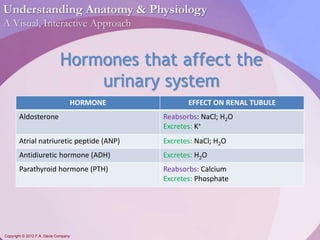
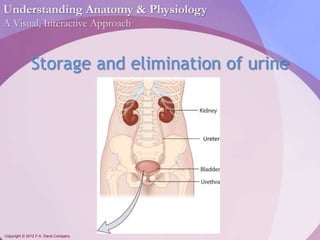
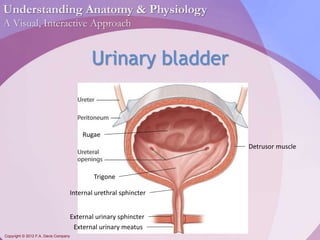
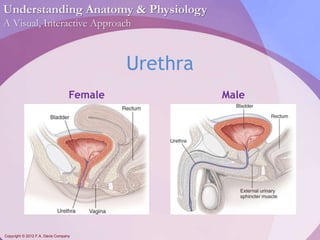
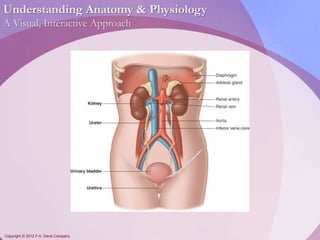
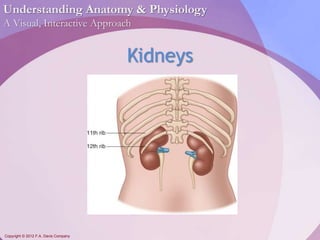
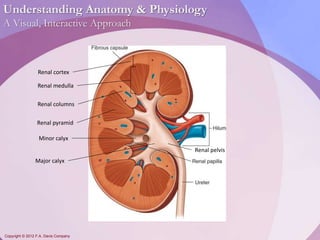
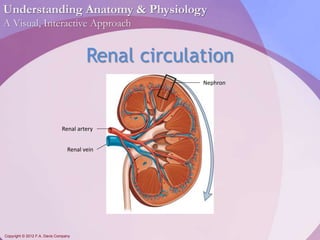
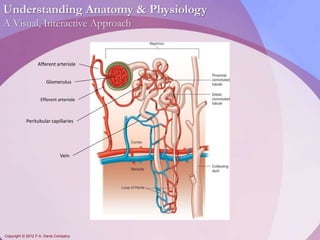
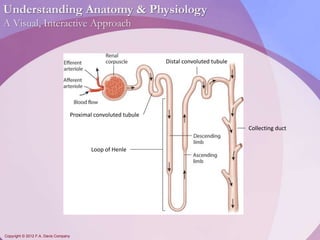
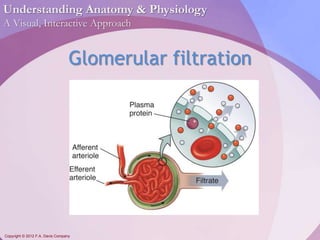
This document discusses the structure and function of the urinary system. It describes the major components, including the kidneys, nephrons, ureters, bladder, and urethra. The kidneys filter waste from the blood to form urine via nephrons and glomerular filtration. Urine is transported from the kidneys to the bladder via ureters and stored in the bladder before being excreted through the urethra. Hormones like aldosterone and ADH regulate fluid and electrolyte balance during urine production and excretion.
![Understanding Anatomy & Physiology
A Visual, Interactive Approach
Copyright © 2012 F.A. Davis Company
Regulation of GFR
Glomerular filtration rate [GFR] should be
constant, despite changes in blood
pressure.
If flow is too high, the body will lose
excessive water and nutrients.
If flow is too low, tubules may reabsorb
toxins.](https://image.slidesharecdn.com/chapter18-140829104945-phpapp02/85/Chapter18-Urinary-System-15-320.jpg)