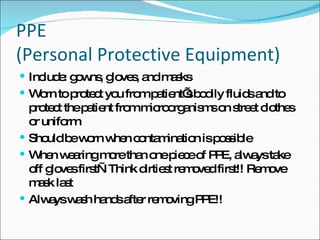
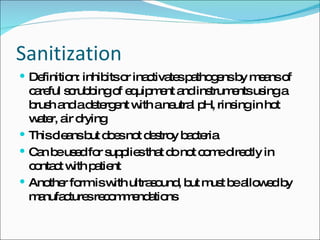
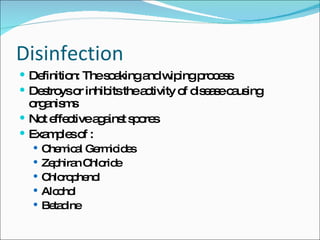
The document defines asepsis as the destruction of organisms after they leave the body. It discusses aseptic techniques like hand hygiene, wearing gloves and PPE, and using clean sterile supplies to prevent the transfer of pathogens. Surgical asepsis maintains a sterile environment to prevent microorganisms from entering the body through sanitation, disinfection and sterilization. The three steps to achieve sterility are sanitization, disinfection and sterilization which clean, destroy bacteria and kill all microorganisms respectively. Autoclaving uses steam pressure and dry heat to sterilize instruments and has time requirements depending on the item.