Modern perioperative fluid management
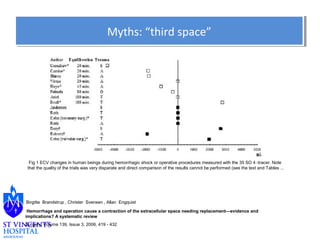
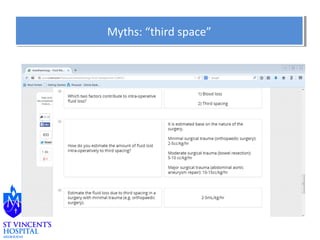
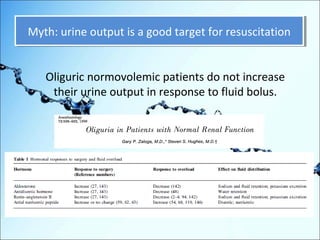
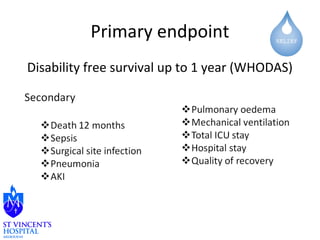
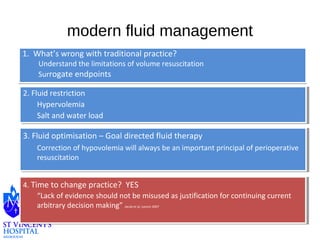
1. What's wrong with traditional practice? Traditional practices rely on surrogate endpoints for fluid resuscitation that have limitations.
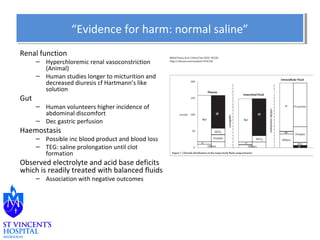
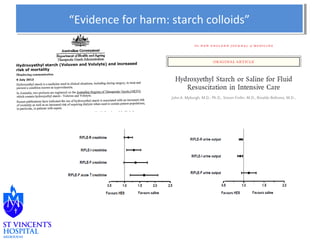
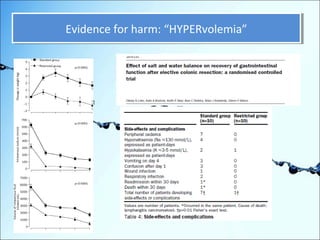
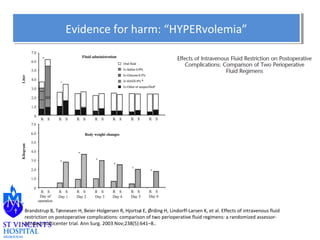
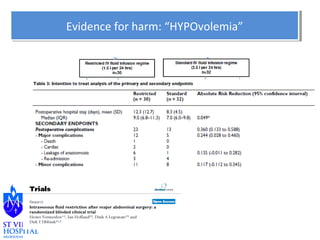
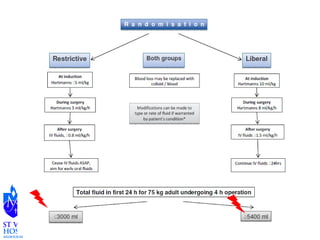
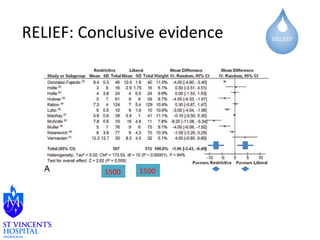
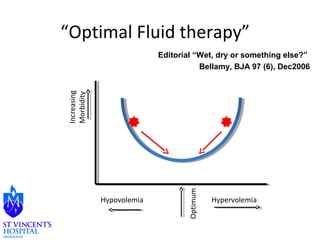
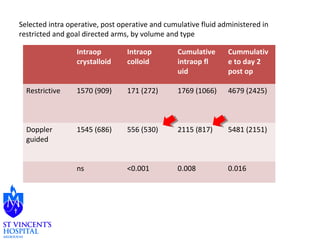
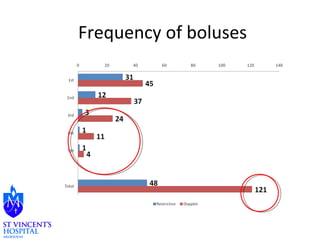
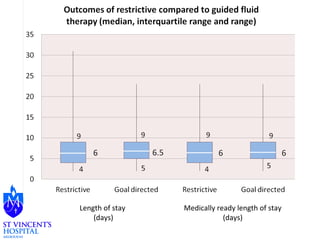
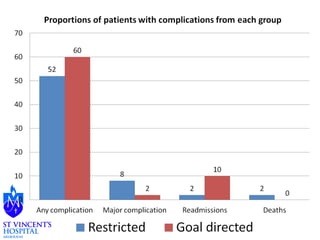
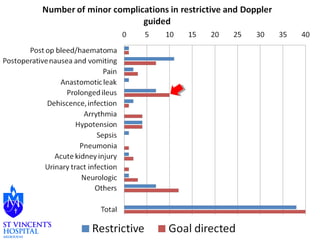
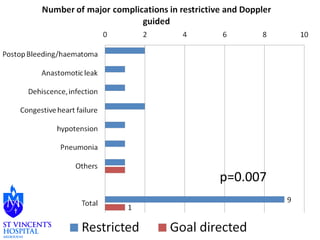
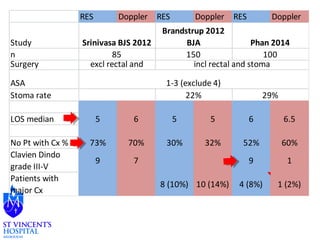
2. Fluid restriction. Evidence shows hypervolemia from excessive fluids can cause harm through salt and water loads.
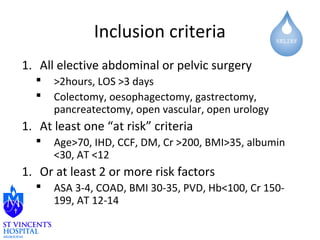
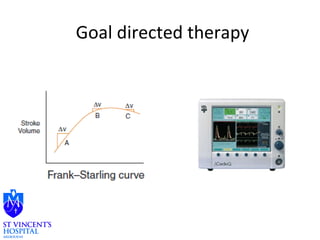
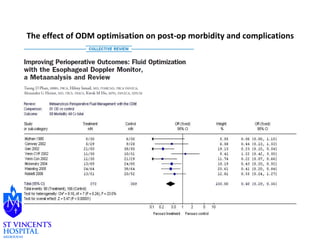
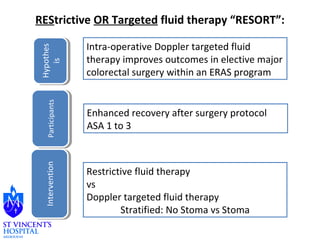
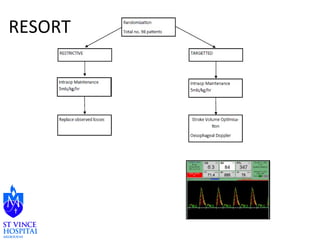
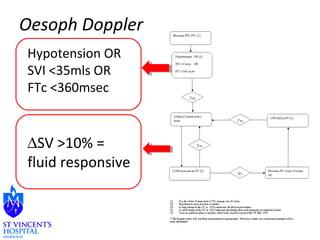
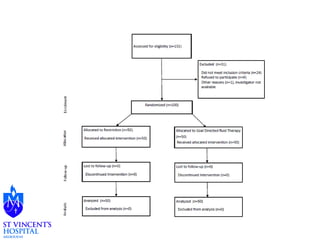
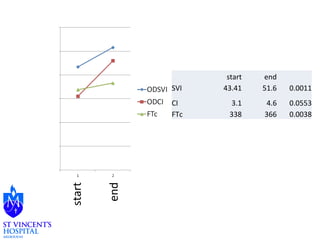
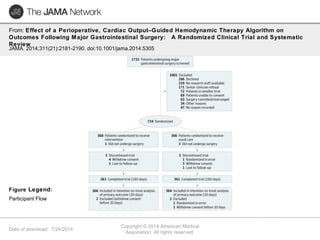
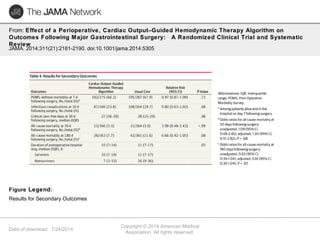
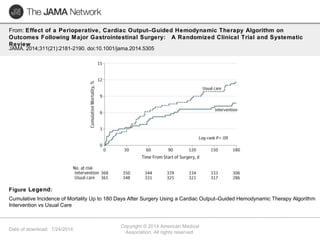
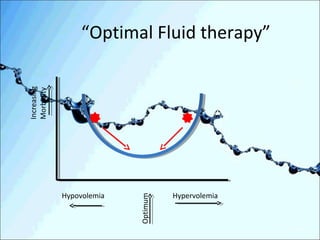
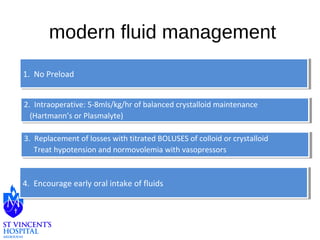
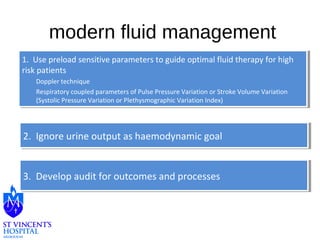
3. Fluid optimisation and goal directed fluid therapy. Using preload-sensitive parameters to guide optimal fluid therapy for high-risk patients, while still correcting hypovolemia which is important for resuscitation.
4. Time to change practice? The evidence calls for a change in practice away from arbitrary decision making toward optimized, goal-directed fluid management.