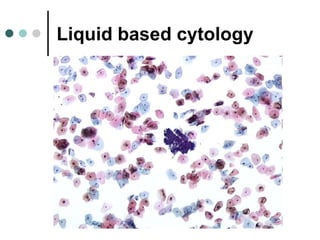
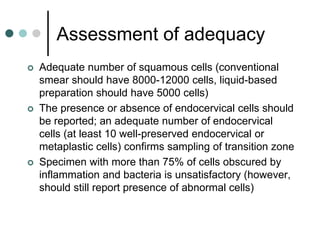
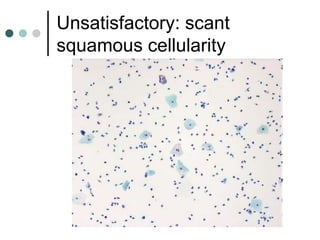
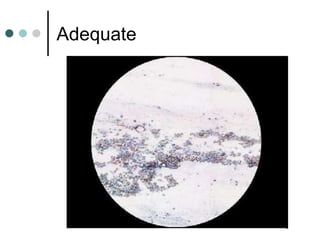
1) The document describes the Bethesda System for reporting cervical cytology results, which standardizes terminology for specimen adequacy, interpretation, and epithelial cell abnormalities.
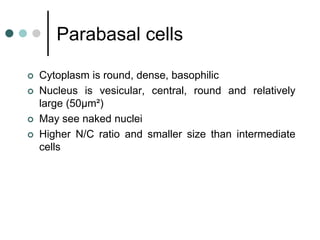
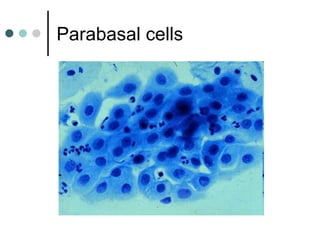
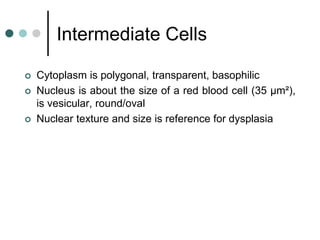
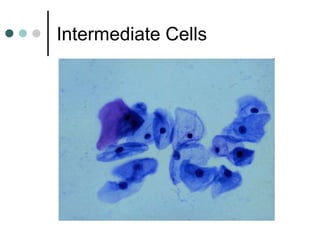
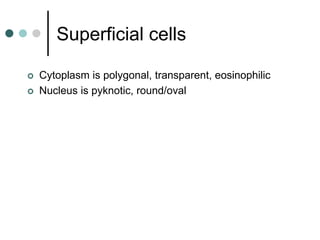
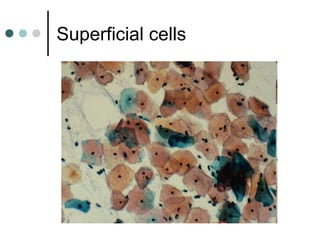
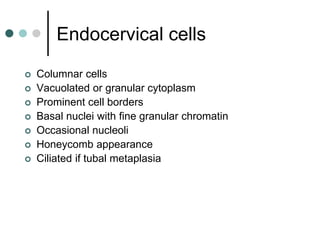
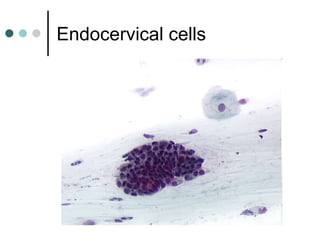
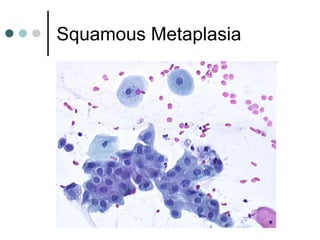
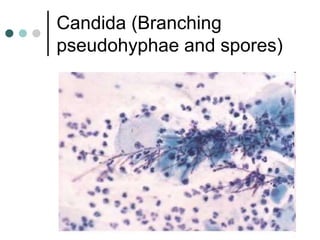
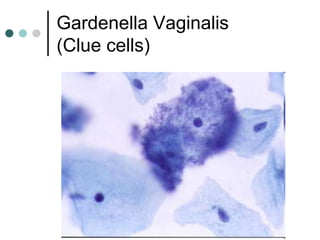
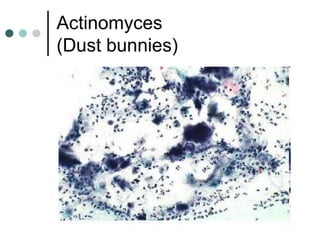
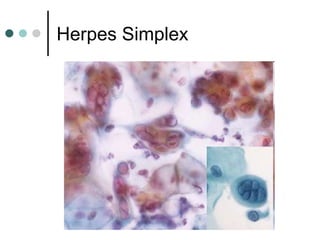
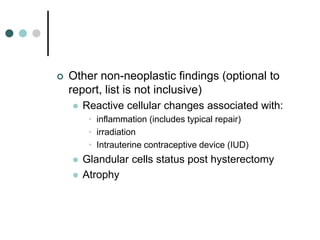
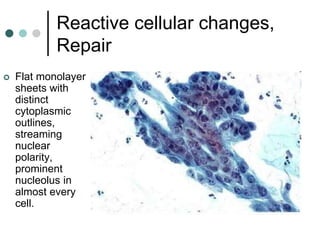
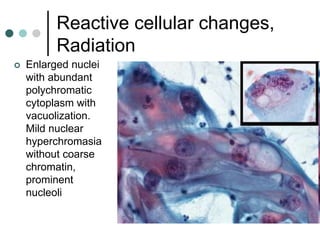
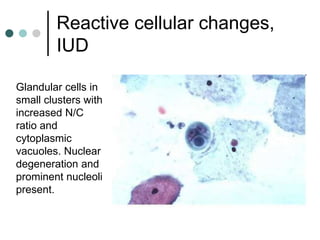
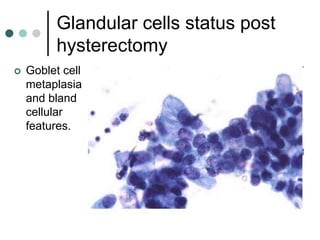
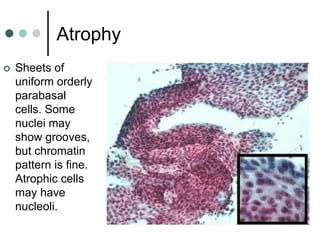
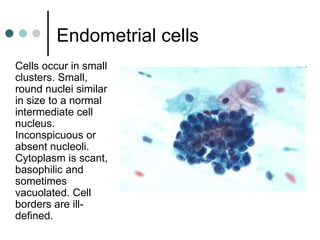
2) Key cell types of the cervix are described along with non-neoplastic and reactive findings like organisms, inflammation, and hormonal changes.
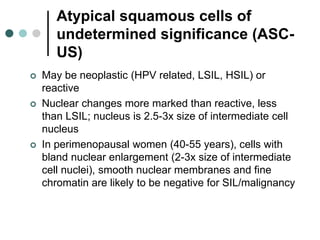
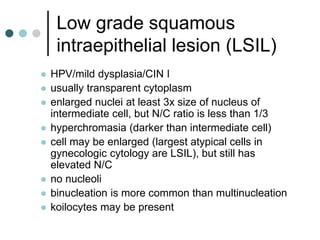
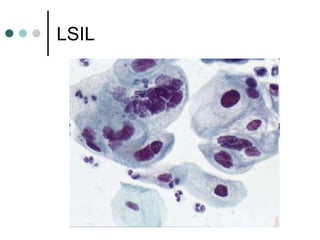
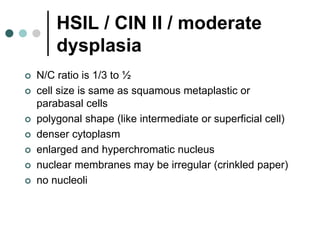
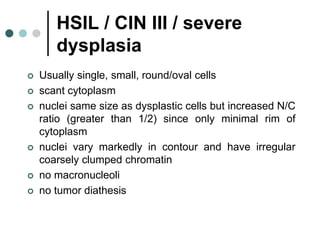
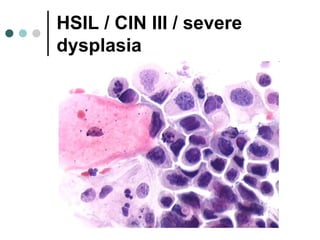
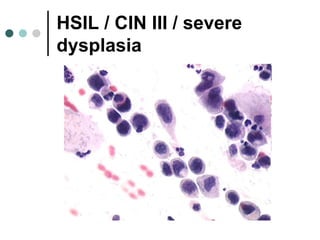
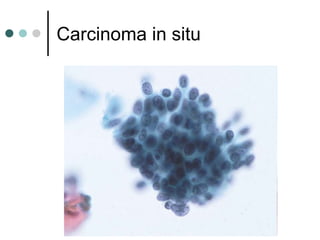
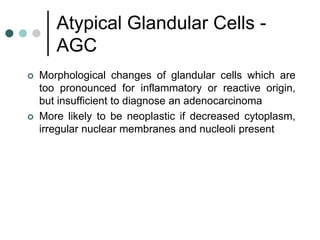
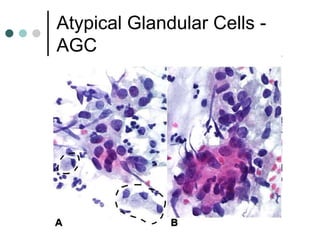
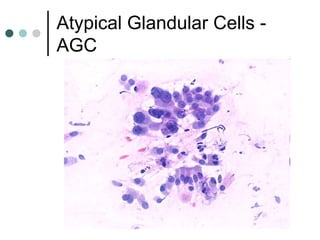
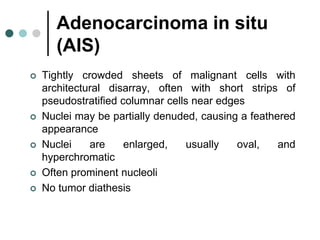
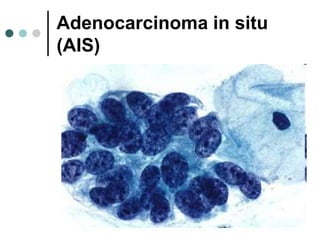
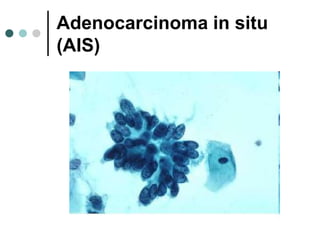
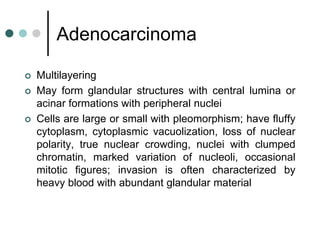
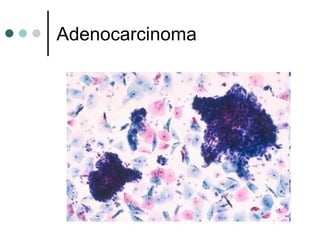
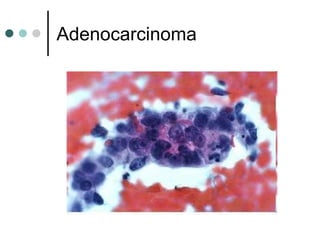
3) Epithelial cell abnormalities are classified as either squamous or glandular, ranging from atypical/precancerous lesions to carcinoma. Nuclear and architectural criteria are provided to distinguish between low and high-grade squamous intraepithelial lesions.